Hand & Wrist Surgery

Our hand surgery service at Hannover Medical School focuses on the diagnosis and treatment of all hand disorders and conditions. Our hand surgeons are plastic and reconstructive surgeons who have received specialized training in hand surgery and are vastly experienced in all types of reconstructive procedures. We offer comprehensive and individualized treatments to tackle even the most complex of cases.
- Carpal tunnel syndrome
- Carpometacarpal joint (CMCJ) arthritis
- Ganglion cyst
- Trigger Finger
- Rheumatoid arthritis
- Dupuytren’s contracture
- Reconstruction of congenital hand malformations such as:
- Syndactyly
- Polydactyly
- Clinodactyly
- Pollex flexor congenitus
- Surgery of the wrist (Carpus) in traumatic and degenerative conditions
- Flexor tendon injury and reconstruction
- Acute trauma care (replantation) and reconstruction of complex hand injuries
- Wrist arthroscopy
Our hand service also has specially trained hand therapists to assist in rehabilitation therapy, splint fabrication and functional evaluation of hand surgery patients.
Hand surgery
Severe injuries to the hand (so-called complex hand injuries) are caused by the use of great force in industrial accidents or DIY work. Often many anatomical structures such as muscles, bones, tendons, nerves, blood vessels and the skin are injured at the same time. This results in comminuted fractures, contusions and, in the case of circular saw injuries, amputation of limbs. In the event of such a serious injury, immediate presentation at a hand surgery center is necessary in order to perform immediate hand surgery. Our Clinical Department's hand surgery center has a full surgical team on call 24 hours a day, 365 days a year, under the direction of an experienced senior physician.
The reconstruction of serious injuries to the hand or arm usually requires several surgical steps. Firstly, in an emergency situation, the survival of the limb is ensured by restoring the blood supply and treating the other functional structures. Further operations are often necessary to clean the wounds, usually due to more severe contamination, until finally, in the case of exposed functional structures, a plastic defect can be covered with a skin-muscle flap. In the meantime, the exposed structures can be protected from infection with various special dressings (e.g. vacuum dressings).
It is not uncommon for functional deficits to remain due to the severity of the injury, which are subsequently corrected by further plastic reconstructive surgery.
A successful reconstruction is followed by an intensive rehabilitation program, which we start early in the postoperative period. A rehabilitation program in a hand surgery rehabilitation Clinical Department is arranged for patients via our social services, and possibly also through the employers' liability insurance association. In addition, our occupational therapists fit special hand-made splints.
As with arm and hand treatment, complex leg injuries or amputation injuries to the foot are also treated in our Clinical Department.



Structural disorders in the carpus are often caused by accidents involving great force, such as ladder falls, car collisions, accidents at work with heavy tools, falls on black ice or during sport.
The cause is the tearing of ligament structures within the carpus, which then leads to a displacement of the carpal bones and consequently to cartilage damage in the wrist area.
Various reconstruction options are available depending on the extent and pattern of the damage. On the one hand, we carry out reconstructions on the wrist using the existing ligaments, direct ligament sutures or replacement plasty (wrist capsule, ligaments), usually with the simultaneous insertion of temporary metal pins. These metal pins are left in place for a few weeks and can then be removed as part of an outpatient operation.
Partial stiffening operations are also an option. Here, individual carpal bones are locked together to prevent the bones from moving further apart and cartilage damage from progressing. The aim is to maintain maximum mobility of the hand. In some cases, it is necessary to remove individual carpal bones in combination with a partial stiffening operation. A piece of bone from the iliac crest or the radius is inserted into the carpal block and secured with metal pins or metal plates.
Following the operation, the patient is immobilized in a plaster cast for several weeks and the metal pins are removed in a short operation if there is X-ray evidence of firm bony development. This is followed by intensive physiotherapy treatment to regain mobility, whereby a reduction in the range of motion is to be expected after partial carpal fusion surgery. As an alternative to partial fusion of the wrist, in certain cases of wrist arthrosis we offer partial removal of the carpal bones in order to achieve pain-free or at least low-pain residual mobility for our patients with a shorter procedure and a shorter post-operative immobilization period.
Another surgical option is the complete fusion of the carpus in severely damaged cartilage surfaces. Here too, a bone block is removed from the iliac crest, inserted into the carpus and fixed with a metal plate. A complete stiffening of the wrist is followed by several weeks of immobilization in plaster, whereby the metal plate is not removed.
Occasionally, operations that eliminate pain alone are an effective treatment option.
These operations are performed during an inpatient stay of approx. 1 week. As soon as the arm has swollen down after the operation, we can apply a light plastic cast with which the patient leaves the hospital. A post-operative X-ray is taken before the patient is discharged.

Flexor tendons transmit the force of the forearm flexor muscles to the wrist and fingers. They run on the flexor side of the forearm and pass through a narrow tunnel, the so-called "carpal tunnel", at the level of the carpus into the palm and from there to the individual fingers. Each finger is moved via a superficial and deep flexor tendon. This enables the complicated movements of the wrist and finger joints.
Possible causes of flexor tendon injuries are lacerations and cuts, degenerative or infection-related injuries. The diagnosis is made clinically by testing the flexor function and, in individual cases, also by means of ultrasound or cross-sectional imaging (magnetic resonance imaging: MRI).
The flexor tendon is surgically reconstructed within the first 6 hours after the injury via a zigzag-shaped incision on the inside of the fingers in the direction of the palm.
If a tendon suture is possible, this is performed using a core suture with fine adaptation.
If both flexor tendons have been severed several weeks ago or extensive destruction has occurred (e.g. due to milling, circular saws, explosions), the injury is treated by means of tendon transplantation. The aim here is to relocate sutures at risk of adhesions to unproblematic areas, e.g. the distal phalanx, palm and forearm near the wrist. This surgical procedure is also indicated for failed primary reconstruction attempts and after healing tendon sheath phlegmon.
The prerequisites for this are wounds that have healed without irritation and good passive mobility of the joints.
The follow-up treatment requires special attention. The initially tight tendon suture initially loses its tensile strength between the 1st and 2nd postoperative week in particular, before gaining strength again after the 2nd week due to healing processes. Nevertheless, the risk of rupture in the suture area is still relatively high up to the 8th week. Prolonged follow-up treatment is therefore strongly recommended.

Congenital malformations of the hands are rare. The severity of a malformation can range from very mild, purely "cosmetic" to severe functional impairments. An early consultation with a hand surgeon is advisable to discuss the need for treatment, timing and prognosis. Many fears of affected parents and children can be allayed during a consultation.
Many different causes can lead to disorders during the hand development of an embryo and thus cause hand malformations of varying degrees. One major factor is genetic changes that can lead to maldevelopment of the hands or feet. These genetic changes may have had an isolated influence on the development of the hands or individual fingers or may affect other organ systems and also the hands as part of complex malformation syndromes. It is also important to look for any other affected individuals in the family when clarifying a hand malformation, as a risk of recurrence for other siblings or children of the affected person can be assessed. We recommend contacting our human geneticists for this purpose.
Below we present some examples of hand malformations from our Clinical Department. In the vast majority of cases, good to very good results can be achieved for the children using modern hand surgery procedures.
Pollex flexus congenitus (congenital flexed thumb)
Children are unable to actively extend their thumb. This rather common deformity is often overlooked in the first few months of life and is caused by an excessively tight ligament at the base of the thumb, which guides the thumb flexor tendon. In a short operation, the frenulum is split through an incision just a few millimetres long, thus permanently eliminating the functional disorder.
Syndactyly (fused fingers)
If 2 or up to 5 fingers are fused together, a purely "membranous" syndactyly must be distinguished from a bony syndactyly. The individual fingers may be completely normally developed apart from a membranous fusion or may also exhibit developmental disorders such as fingers that are too short, symbrachidactyly or missing phalanges.
Polydactyly
The number of fingers may deviate from the norm. In this case, additional underdeveloped fingers may be present, which can be treated non-surgically by tying off a painless suture and waiting for the finger to drop spontaneously. In some cases, however, surgical interventions are also necessary to enable optimal function and development of the affected hand. Here it is important to analyze precisely before and during the operation which finger is additionally attached and therefore needs to be removed.
Malformations of the thumb are of particular importance, as impaired function or even the absence of a thumb significantly impairs hand function. Only the thumb enables the human hand to perform differentiated motor functions.
The double thumb is a special form of polydactyly of the thumb. In this case, the supernumerary part is removed, possibly in combination with a repositioning of the regularly formed but malpositioned thumb into the correct position.
If the thumb is completely missing, this is the most severe form. In this case, a thumb must be recreated. This can be done by moving the index finger into the thumb position (pollicization) or a complete reconstruction from a microsurgically transplanted second toe of the foot.
In clinodactyly, which usually only affects the little finger, the distal phalanx is angled more towards the thumb. If necessary, corrections can be achieved surgically by straightening the middle phalanx.
Other types of malformation and combinations of different malformations are possible. If you have any further questions, we will be happy to advise you in a detailed consultation in our special consultation hours. During a personal consultation, we can then explain the exact surgical steps and types of aftercare. Splint treatment is often necessary. Various corrective procedures can be combined in the case of complex deformities. In some cases, both bony and soft tissue reconstructions must be carried out at the same time. Operations in several stages may be necessary.

The clinical picture first described by Baron Guillaume Dupuytren 160 years ago is a nodular or extensive change in the connective tissue on the inside of the hand with a tendency to form coarse cords that force the fingers to bend.
The ring and little fingers are most frequently affected, predominantly in men in the 4th and 5th decade of life.
Many different triggering causes are currently being discussed, such as chronic mechanical stress, injuries, alcoholism or diabetes mellitus. A familial accumulation in several generations is undisputed.
The diagnosis of this disease is based on a detailed clinical examination.
A special feature is that recurrence or symptoms can also occur on other fingers or the thumb.
We recommend a wait-and-see approach for mild cases. Surgical measures may be considered in cases of rapid progression and functional impairment.
Surgical treatment, with the lowest recurrence rate, is still the most sustainable method.
Our standard procedure consists of using a microsurgical technique, i.e. magnifying glasses, to selectively remove altered connective tissue via zigzag-shaped skin incisions in the palm of the hand while sparing blood vessels and nerves.
An alternative is percutaneous needle fasciotomy. However, this is only possible if the initial disease is not too pronounced. The altered connective tissue is not removed and the success of the operation is often not permanent. The finger can also be straightened by enzymatic thickening of the cord using collagenase injections with the drug Xiapex. Further information on this can be found in the following text.
In advanced stages, additional measures such as joint release or joint stiffening (by inserting wire pins) may be necessary. If necessary in combination with local skin flap plasty.
A compression bandage and a plaster splint are applied immediately after the operation.
Depending on the severity of the disease and the accompanying illnesses, the operation is performed under outpatient or usually inpatient conditions.
Afterwards, regular dressing changes and wound checks by the doctor providing further treatment are required. The suture material inserted can be removed on the 14th postoperative day.
Aftercare is of great importance for the best possible surgical result. Intensive physiotherapy and occupational therapy, as well as nightly splint immobilization to prevent a recurrence of contracture, are essential.
Injection of collagenase (Xiapex ©) for Dupuytren's disease
Since May 2011, following positive admission of the drug in the USA by the FDA, Xiapex has also been approved in the EU as a drug for the treatment of advanced single-strand Dupuytren's disease.
The Enyzm, which is able to break down collagen, is injected directly into the scarred connective tissue strand and leads to the dissolution of this strand. 24 hours after the injection, the affected finger is stretched by the practitioner, thus breaking up the scarred Dupuytren's cord.
Both the collagenase injection and the manual solution should only be carried out by hand surgeons certified by the manufacturer.
Patients with second to third degree Dupuytren's disease with a cord in the palm are potential candidates for the procedure. Collagenase injection is not a promising treatment for cords that cross the PIP joint.
Cost coverage should be clarified with the relevant health insurance company before treatment.
Further information about Dupuytren's disease and treatment with collagenase, including from those affected, can also be obtained from the Dupuytren's self-help association at

Carpal tunnel syndrome (CTS) is caused by pressure on the median nerve in the carpal tunnel at the wrist.
The median nerve runs in the carpal tunnel together with the finger flexor tendons and can be affected by many different causes. These include degenerative, systemic (polyarthritis), metabolic (diabetes) and inflammatory diseases. Wrist injuries, pregnancy or tumors can also trigger CTS.
Most patients suffer from numbness, particularly in the thumb, index finger and middle finger. In addition, there is often a feeling of swelling in the hand and pain that wakes the patient up at night and prevents them from sleeping. The symptoms can radiate to the upper arm and shoulder. As the condition progresses, objects slip out of the patient's hand as the sensory disturbance prevents a permanent and strong "grip". Finally, muscle wasting in the thumb and involvement of the flexor tendons make finger movements very laborious.
Depending on the severity of the condition, various therapeutic measures can be considered. The affected hand is immobilized with a splint at night.
Local cortisone therapy can be used to treat a reactive inflammatory change in the tendon gliding tissue.
The surgical opening of the carpal canal relieves the pressure on the nerves and usually leads to noticeable relief immediately after the operation. This procedure can be performed in our outpatient surgery center under local anesthesia.
For open surgical treatment, the carpal roof (flexor retinaculum) is completely split via an approx. 4 - 5 cm long incision in the palm. At the end of the operation, a plaster splint is applied for a few days. The suture material is usually removed 12 to 14 days after the operation. As a rule, follow-up treatment can be carried out by the referring specialist or general practitioner. The entire treatment period usually lasts two weeks.
During this period, the operated arm should be elevated to avoid increased swelling. Full extension and flexion of all fingers should be ensured as early as one day after the operation.

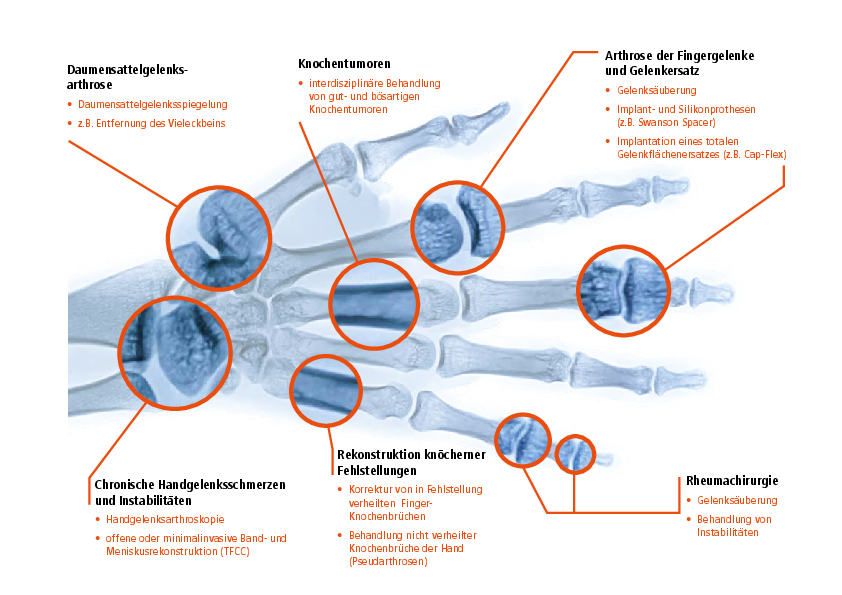
The common so-called rhizarthrosis of the thumb saddle joint is caused by wear and tear of the joint cartilage and occurs in isolation on one or both hands. A familial disposition has been observed. Women are affected more often than men.
Osteoarthritis in the thumb saddle joint progresses through various stages, resulting in a very painful restriction of movement with morning stiffness in the early phase, which improves during the course of the day. As the disease progresses, any movement of the thumb becomes very painful, resulting in a serious loss of hand function. The reason for the pain is the rubbing together of the 1st metacarpal bone and the "large polygonal bone" (Os trapezium). The disease is diagnosed after a thorough clinical examination and confirmed by X-ray.
Conservative treatment through immobilization, possibly in combination with injection treatments, unfortunately only rarely leads to a lasting improvement in the symptoms. Surgical treatment is therefore often the only way to end the pain.
The standard procedure in our Clinical Department is to remove the "large polygonal bone" (Os trapezium) so that the small distance between the bones rubbing against each other is eliminated. If the saddle joint is unstable due to advanced findings, we perform a so-called resection arthroplasty according to Epping. In this procedure, we remove the trapezium and stabilize the joint with a tendonplasty (halved tendon of the flexor carpi radialis muscle).
As a rule, a short inpatient stay is necessary.
After the operation, the thumb is immobilized in a plaster splint for a total of 6 weeks. The other long fingers can be exercised during this time.
From the 4th week of thumb immobilization, active movement exercises (e.g. spreading and bringing the thumb closer) can be started under physiotherapeutic guidance. Powerful and pain-free use of the affected hand can only be expected in 4 - 6 months.

A ganglion, also known colloquially as a ganglion, is a benign tumor formation on the hand that originates from either the joint capsule or a tendon sheath.
Despite its often hard-to-touch consistency, it is not a bone. A genuine bony neoplasm is referred to as an exostosis.
The causes are varied: chronic irritation (joints, tendon sheaths) as well as injuries (rupture of the joint capsule) can play a role.
The bulging elastic distension usually contains a viscous mucus, can grow to a considerable size and causes discomfort due to pressure on neighboring structures such as skin, nerves, vessels or tendons.
On the finger, a special form, the so-called mucoid cyst, leads to nail growth disorders (ridges) due to pressure on the nail bed.
The diagnosis of a ganglion can usually be made by an experienced hand surgeon through a clinical examination. Sonography and X-rays may also be necessary.
Treatment is usually surgical, whereby the ganglion must be completely removed together with the stalk, which is often present, in order to prevent recurrence.

This particular disorder usually affects the first annular ligament of the finger flexor tendons.
The phenomenon can occur congenitally in infants, occasionally in small children, but in the majority of cases in adults over the age of 50. Possible causes are repeated overuse or chronic inflammatory diseases such as gout, rheumatism or other diseases such as diabetes mellitus.
In adults in particular, this is a thickening of the tendon or the tendon gliding layer, so that the diameter of the annular ligament is no longer sufficient for the tendons to glide undisturbed. This causes the finger to "get stuck", so that the painful blockage in movement can only be overcome with increased force or by using the other hand.
The condition can usually be diagnosed on the basis of a thorough clinical examination.
In the early stages without actual snapping during finger movement, conservative treatment with local decongestant measures and anti-inflammatory medication, possibly cortisone injections into the tendon sheath, is possible.
However, surgical splitting of the annular ligament should be performed at an early stage, before fixed movement restrictions have already occurred. The snapping symptoms disappear immediately after the operation.
In order to achieve an optimal surgical result and to prevent adhesions or adhesions of the flexor tendons, the fingers must be exercised independently from the day of surgery after a brief instruction.
In difficult cases, e.g. if finger mobility is restricted, physiotherapy and occupational therapy exercises are possible. The skin sutures can be removed in two weeks by the doctor providing further treatment.
Ring ligament splitting can be performed under local anaesthetic in our outpatient surgery center.

Rheumatoid arthritis (RA; formerly known as chronic polyarthritis; cP) is a chronic inflammatory (abacterial) systemic disease that primarily affects the synovial membrane (synovium) and leads to pathological changes in joints and tendons. It affects 1-4% of the population in Germany. Women between the ages of 40 and 60 are most frequently affected.
The exact reasons for the development of RA are still unknown. Many of the pathological findings point to an autoimmunological background. Another theory assumes that enzymatic processes are involved in the destruction of joint structures and tendons. The chronic inflammation, together with enzymatic processes, leads to destruction of the joint structures and ultimately to rupture of the tendons due to the simultaneous presence of tendon sheath synovitis.
At the beginning of the disease, there is morning stiffness of the joints with general symptoms such as tiredness and fatigue. As rheumatoid arthritis is a dynamically progressive disease, swelling of the joints, joint misalignment and finally function-impairing joint destruction can occur as the disease progresses. This results in extremely painful and functionally restricted joints and clearly visible axial deviations with grotesque deformities, e.g. of the hands.
Nerve constriction syndromes are frequently observed, for example carpal tunnel syndrome or compression of the ulnar nerve due to synovitis of the elbow joint. The hands are affected in almost all rheumatism patients, often in the early stages, typically the wrist, the metacarpophalangeal and metacarpophalangeal joints of the fingers and the metacarpophalangeal joint of the thumb.
The important rheumatic changes in the hand are briefly described below:
Changes in the wrist
In the early stages, pain and restricted movement indicate wrist synovitis, which can be felt as a bulging swelling.
Depending on how it progresses, spontaneous stiffening of the wrist or function-restricting instability may occur in the later stages.
Changes to the finger joints Swan neck deformity
In this deformity, the metacarpophalangeal and metacarpophalangeal joints are held in flexion and the middle joint in hyperextension, which impedes fist closure and the fine pointed grip between the thumb and the affected finger. This is caused by rheumatic changes in the joints, the palm muscles and the flexor tendon sheaths.
A "snapping phenomenon" can also occur: When the fist is closed normally, the finger remains in a hyperextended position. When flexion is increased, the middle phalanx is pulled over the head of the proximal phalanx, resulting in a typical snap. Only now is it possible to close the fist.
Buttonhole deformity
Synovialitis stretches and loosens the middle phalanx of the extensor apparatus and weakens the extension of the middle joint. The connective tissue membrane (aponeurosis) between the medial and lateral phalanges widens, the lateral phalanges slip towards the inside of the hand and now act as flexors in the medial joint and extensors in the distal joint.
Changes to the saddle joint of the thumb
Arthritic changes to the saddle joint of the thumb are very common, which lead to severe pain even when gripping firmly, grasping a key or holding a coffee cup. This results in a significant reduction in strength.
Therapy
As RA is a progressive general disease, surgical treatment must be carried out in close consultation with the treating rheumatologist. For example, immunosuppressive medication should be reduced to a minimum before a planned operation, as otherwise there is a risk of wound healing disorders.
The aim of surgical treatment in the early stages is to
- slowing down the disease process,
- Reduction of pain,
- improve or restore useful functions,
- prevention of progressive destruction and
- improving the aesthetic appearance.
The 3 basic principles are
- Prevention of progressive destruction through synovialectomy,
- restoration of lost functions and
- Interventions to preserve residual functions, e.g. arthroplasty or tendon surgery.
Preventive operations include synovialectomies, which should be performed at an early stage to prevent impending tendon ruptures. Reconstructive measures aim to restore the soft tissue mantle and joints (also by inserting artificial joints) and e.g. tendon displacements. In addition, resection arthroplasty with tendon plasty is carried out for saddle joint arthrosis, for example. In cases of advanced instability with skeletal collapse, fusion is indicated in order to preserve residual hand function.
In general, preference should be given to procedures that are as simple as possible, with minimal stress for the patient, a short rehabilitation period and a high chance of success.

Since the development of the smallest, most powerful instruments and video units with high resolution, wrist arthroscopy has enriched diagnostics and minimally invasive treatment of selected wrist procedures.
It is used in particular as follows
- Clarification of unclear complaints in the wrist that cannot be diagnosed using non-invasive methods (e.g. X-ray, CT, MRI).
- for fresh wrist injuries with swelling without pathological radiological findings and suspected ligamentous injury
- Minimally invasive removal of free joint bodies
- Smoothing of cartilage lesions and cartilage parts.
- Smoothing of impacted and often injured parts of the disc after a tear.
As part of an arthroscopy, a camera and a tactile hook or other surgical instruments are inserted into the wrist via 4 small incisions in the skin. Arthroscopy can be performed under arm anesthesia (plexus anesthesia) or under general anesthesia, usually as an outpatient procedure. After the arthroscopy, these areas are sutured or taped with a special plaster.
The first dressing is changed on the first or second day after the arthroscopy. Depending on the injury and treatment, the wrist is either immobilized in a splint or can be mobilized immediately. Physiotherapy exercises are rarely necessary.
We will be happy to discuss the findings and in particular the next steps with you in our outpatient clinic.
DGPRÄG: Hand surgery
The German Society of Plastic, Reconstructive and Aesthetic Surgeons (abbreviation: DGPRÄC) is a professional association and the scientific society for plastic surgeons in Germany, based in Berlin. The DGPRÄC was founded on October 16, 1968 in Bochum under the name "Vereinigung der Deutschen Plastischen Chirurgen" (VDPC), which was adapted in 2005. Members of the DGPRÄC are exclusively specialists in plastic surgery or plastic and aesthetic surgery.