AG Nayak

Chromatin and SUMO physiology group
Research focus
Mobility is an indispensable feature that determines survival and success in the animal world. Skeletal muscle- that allows this mobility- is an astounding organ constituting over 650 muscles accounting for approximately 40% of total body mass and up to 30% of basal energy expenditure. The skeletal muscle displaying a characteristic striated pattern is an array of linearly arranged units called ‘sarcomeres’. The individual sarcomere hosts highly organized structures including the actin, and myosin filaments. The cyclic interaction between these two types of filaments is responsible for generation of force and movement at the molecular to organismic level.
Precise molecular arrangement of sarcomere is central to the muscle function. Importantly, disorganization of sarcomere and thereby defective muscle function are the typical hallmarks of myopathies including cancer cachexia, prevalent in nearly 80% of cancer patients with reported mortality rate in more than 30% patients.
The major focus of our group is understand how SUMO (Small Ubiquitin-like Modifier)-mediated epigenetic program regulates skeletal and cardiac muscle physiology including sarcomere organization, muscle differentiation and regeneration process and muscle wasting diseases such as cachexia. Other major aim of our group is to understand the molecular mechanism of chemotherapy-induced cachexia. Our ongoing projects has established unbiased screening systems to test effects of various chemotherapeutic drugs on muscle wasting with an objective to identify a better therapeutic option that will reduce cancer burden without triggering loss of muscle mass and function.
Lab Projects
- Modulation of chromatin organization by SUMO pathway in myofibril assembly
- Epigenetic signaling in muscle atrophic condition/Cachexia
- Mechanism underlying chemotherapy-induced cachexia
- SUMOs in cachexia and muscle cell metabolism
Lab Members
Principal Investigator: Arnab Nayak
PhD Student: Katharina Brandt
PhD student: Amel Nassar-Grioua
PhD student: Mugeng Li
PhD student: Baoyu Zhou
Technical assistant: Stefanie Nedel
Previous lab members
-
Gand, Luis (now Faculty of Sport and Health Sciences University of Jyväskylä, Finland)
Dr. rer. nat., Molecular mechanisms underlying skeletal muscle wasting in cancer-induced cachexiaKhan, Bushra (now Department for Biochemistry and Molecular Biology, University of Southern Denmark (SDU))
PhD, Molecular insights underlying tyrosine kinase inhibitor-triggered cachexia
How cancer messengers destroy the muscles
MHH scientists are investigating how pro-inflammatory cytokines intervene in the metabolism of muscles and actively remodel them.
Dr Arnab Nayak, private lecturer, investigates the effect of pro-inflammatory messengers on muscle wasting in cancer.
Cancer patients often lose an excessive amount of weight. This affects up to 80 percent of patients and is mainly due to the loss of muscle mass and fatty tissue. This cancer-induced cachexia (CIC) is triggered by cancer cytokines, i.e. inflammation-promoting messenger substances that the tumor cells themselves emit. It is not uncommon for the heart muscle to be affected, which further weakens the patient. Depending on the type of cancer, CIC is responsible for 20 to 50 percent of all cancer-related deaths worldwide. There is no curative therapy. In order to find an effective treatment approach, a research team led by associate professor (PD) Dr. Arnab Nayak, a scientist at the Institute of Molecular and Cell Physiology at Hannover Medical School (MHH), has been investigating the previously unknown molecular mechanisms associated with CIC. With his "Chromatin and SUMO Physiology" working group, the molecular biologist has shown that the cancer cytokines intervene directly in the metabolism of muscle cells and actively remodel them. They also ensure that the muscle can release less calcium, which impairs muscle contraction, i.e. the active contraction of the muscle. The results have been published in the "Journal of Cachexia, Sarcopenia and Muscle".
Loss of the ability to contract
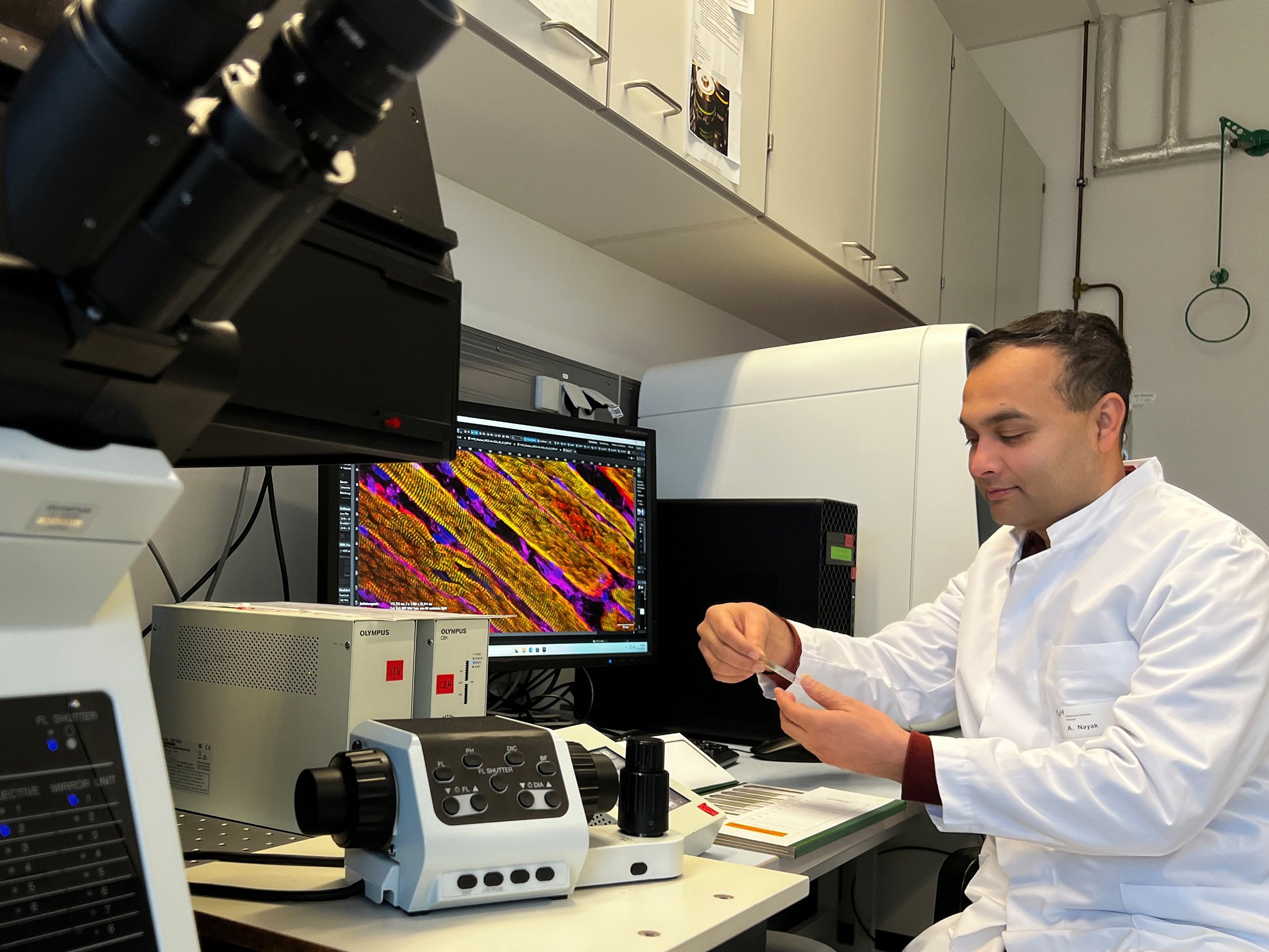
The researchers investigated the effect of CIC on the skeletal and heart muscle cells of mice and rats in cell culture. They tested the contractile properties of the muscle cells after electrical stimulation and measured the release of calcium within the muscle cells. They also used a high-resolution microscope to monitor how CIC affects the organization of the sarcomeres, the smallest functional units of the muscle. They also analyzed the signal transmissions in the cells that regulate which muscle-specific genes are switched on or off. "We observed a drastic loss of contraction of striated muscle cells in CIC, which was primarily due to acutely disorganized sarcomere structures and an impaired calcium transport process," states PD Dr. Nayak.
However, the proinflammatory cytokines not only reduce the muscle's ability to contract. They also destroy the muscle cells themselves. On the one hand, they activate an enzyme that marks muscle proteins for degradation. The system is supposed to remove faulty proteins from the cell. In this case, however, the degradation system ensures that functioning muscle proteins are destroyed. In addition, the cytokines influence a central signaling pathway within the muscle cells that regulates their growth, division, metabolism and survival.
SUMO signaling pathway as a therapeutic approach
Current therapies tend to focus on alleviating the symptoms. For example, dietary supplements such as polyunsaturated omega-3 fatty acids in combination with vitamin D3 and endurance and strength exercises are used in an attempt to stop muscle atrophy. Cardiac medication such as ACE inhibitors or beta-blockers should also help to at least reduce muscle loss. PD Dr. Nayak relies on molecular biological methods, or more precisely, the so-called SUMO signaling pathway. In this mechanism, the protein SUMO (small ubiqutin-like modifier) is bound to other proteins in order to change their function. The SUMO signaling pathway plays an important role in muscle breakdown. The SUMO-specific enzymes SENP3 and SENP7 regulate epigenetic processes in the muscle-specific genes. These control gene activity without changing the DNA itself.
In cachexia, the enzymes are degraded and, as a result, their muscle-specific target genes are downregulated. As a result, the sarcomeres, the smallest functional units of the muscle, can no longer form as intended and the muscles lose their ability to develop strength. "In our study, we upregulated SENP3 and SENP7 and observed a decrease in muscle degradation," says the molecular biologist. However, whether this approach works beyond cell culture still needs to be investigated further. PD Dr. Nayak and his team therefore want to test the muscle-saving effect in a mouse model next.
Text: Kirsten Pötzke
SERVICE:
The original paper "Calcium Handling Machinery and Sarcomere Assembly are Impaired Through Multipronged Mechanisms in Cancer Cytokine-Induced Cachexia" can be found here.
How chemotherapy drug sorafenib causes muscle wasting
Research team clarifies molecular basis for cachexia.
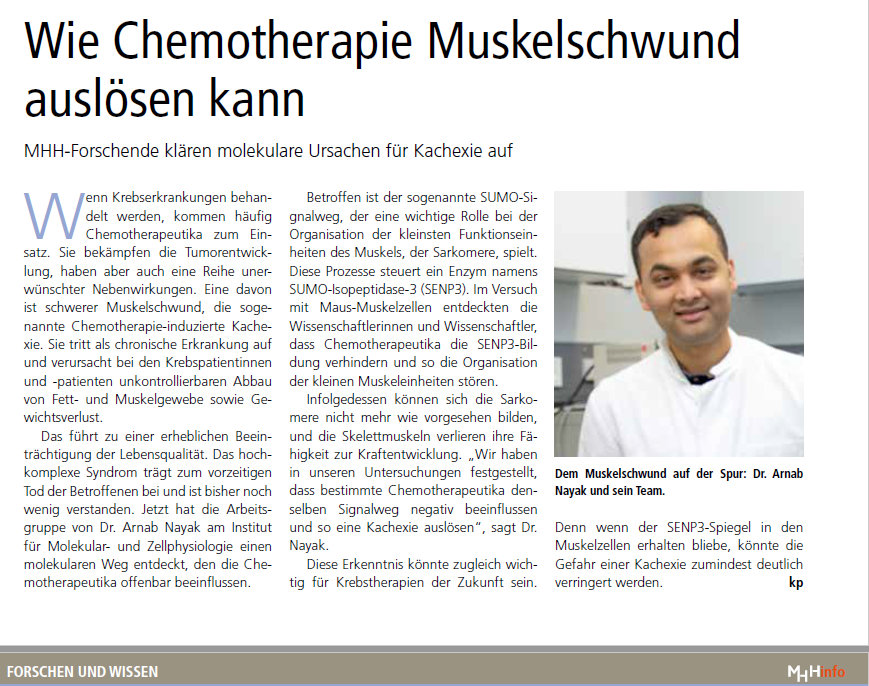
Chemotherapy fights cancer, but can also damage the muscles. Researching muscle atrophy caused by chemotherapy.
Chemotherapeutic agents are often used to treat cancer. They combat tumour growth, but also have a number of undesirable side effects. One of these is severe muscle wasting, known as chemotherapy-induced cachexia. This chronic disease causes uncontrollable breakdown of fat and muscle tissue as well as weight loss. However, in order to improve treatment strategies, the molecular basis must first be understood. This is where PD Dr Arnab Nayak, a scientist at the Institute of Molecular and Cellular Physiology at Hannover Medical School (MHH), comes in. With his research group ‘Chromatin and SUMO Physiology’, the molecular biologist has shown that the chemotherapeutic agent sorafenib actively remodels skeletal muscle cells and thus triggers cachexia. The work has been published in the journal ‘iScience’.
Formation and function of skeletal muscle fibres impaired
Sorafenib is used for liver cell carcinoma (HCC) and renal cell carcinoma (RCC), among others. The chemotherapeutic agent belongs to the so-called tyrosine kinase inhibitors, which attack chemical messengers that are important for tumour development. Sorafenib targets several enzymes involved in cell growth as well as the formation of new blood vessels triggered by the tumour itself, which tumours use to ensure their supply of oxygen and nutrients. At the same time, sorafenib interferes with epigenetic regulation in muscle-specific genes. Epigenetics describes mechanisms that do not influence the genes themselves, but their activity.
In this way, epigenetic processes control which genes are switched on or off and therefore also have an influence on whether and when a disease breaks out or not. Through epigenetic mechanisms, cells react to environmental influences, among other things.
In the case of sorafenib, the researchers have uncovered an unusual molecular mechanism in transcription, i.e. in the reading of the DNA sections relevant to the muscle fibres and their transfer into the corresponding blueprint. In the case of sorafenib, the researchers have uncovered an unusual molecular mechanism in transcription, i.e. in the reading of the DNA sections relevant to the muscle fibres and their transfer into the corresponding blueprint.This leads to impaired development of the skeletal muscle fibres.
Basis for therapeutic fine-tuning
The researchers also investigated the drugs nilotinib and imatinib, which belong to the same class of chemotherapeutic agents. Nilotinib is used in particular for chronic lymphocytic leukaemia (CLL), while imatinib is used to treat acute lymphoblastic leukaemia (ALL) and gastrointestinal stromal tumours (GIST). ‘Interestingly, these two tyrosine kinase inhibitors did not show a similar effect on muscle cell function,’ says PD Dr Nayak. According to the cell biologist, the critical evaluation of cancer-specific chemotherapeutic agents with regard to their effects on muscle physiology is the key to developing better therapies. ‘The detailed findings from our study provide the background and framework for similar future investigations to fine-tune chemotherapeutic treatment. The correct selection of drugs with minimal side effects or potentially harmful effects that can be counteracted is only possible with knowledge of the underlying affected signalling pathways.
Therefore, the implications of these findings for the development of balanced combination therapies for affected individuals to improve treatment are of immediate importance. Nevertheless, sorafenib is currently one of the best therapeutics for the treatment of HCC and RCC. ‘However, our findings have the potential to develop new therapeutic regimens to minimise chemotherapy-induced cachexia,’ says PD Dr Nayak.
The original paper ‘Sorafenib induces cachexia by impeding transcriptional signalling of the SET1/MLL complex on muscle-specific genes’ can be found here.
Text: Kirsten Pötzke
Funding
- Individual research grant from the German Research foundation (DFG). NA 1565/2-1
- Individual research grant from the German Cancer Aid (DKH). Identification no.- 70115510.
Lab Methodologies
To address our scientific objectives, we employ diverse experimental approaches, including quantitative proteomics, SUMO proteomics, CRISPR/Cas9-mediated genome editing tools to check chromatin events of a single gene, epigenomics (ChIPseq, chromosome conformation capture etc.), cell contractility assay, measurement and quantification of calcium transient process and single molecule biophysical methods such as total internal reflection fluorescence microscopy (TIRFM).
Selected publications (*corresponding author)
- Gand LV, Lanzuolo C, Li M, Rosti V, Weber N, Lu D, Bar C, Thum T, Pich A, Kraft T, Amrute-Nayak M, Nayak A* (2025) Calcium Handling Machinery and Sarcomere Assembly are Impaired Through Multipronged Mechanisms in Cancer Cytokine-Induced Cachexia. J Cachexia Sarcopenia Muscle 16: e13776
- Khan B, Lanzuolo C, Rosti V, Santarelli P, Pich A, Kraft T, Amrute-Nayak M, Nayak A* (2024) Sorafenib induces cachexia by impeding transcriptional signaling of the SET1/MLL complex on muscle-specific genes. iScience 27: 110913
- Wang T, Nayak A, Kraft T, Amrute-Nayak M (2024) Single-Molecule Investigation of Load-Dependent Actomyosin Dissociation Kinetics for Cardiac and Slow Skeletal Myosin. Small 20: e2406865
- Spahiu E, Uta P, Kraft T, Nayak A*, Amrute-Nayak M (2024) Influence of native thin filament type on the regulation of atrial and ventricular myosin motor activity. J Biol Chem 300: 107854
- Khan B, Gand LV, Amrute-Nayak M, Nayak A* (2023) Emerging Mechanisms of Skeletal Muscle Homeostasis and Cachexia: The SUMO Perspective. Cells 12
- Amrute-Nayak M, Gand LV, Khan B, Holler T, Kefalakes E, Kosanke M, Kraft T, Nayak A* (2022) SENP7 deSUMOylase-governed transcriptional program coordinates sarcomere assembly and is targeted in muscle atrophy. Cell Rep 41: 111702
- Wang T, Spahiu E, Osten J, Behrens F, Grunhagen F, Scholz T, Kraft T, Nayak A*, Amrute-Nayak M (2022) Cardiac ventricular myosin and slow skeletal myosin exhibit dissimilar chemomechanical properties despite bearing the same myosin heavy chain isoform. J Biol Chem 298: 102070
- Wang T, Brenner B, Nayak A*, Amrute-Nayak M (2020) Acto-Myosin Cross-Bridge Stiffness Depends on the Nucleotide State of Myosin II. Nano Lett 20: 7506-7512
- Amrute-Nayak M, Pegoli G, Holler T, Lopez-Davila AJ, Lanzuolo C, Nayak A* (2020) Chemotherapy triggers cachexia by deregulating synergetic function of histone-modifying enzymes. J Cachexia Sarcopenia Muscle
- Nayak A*, Amrute-Nayak M (2020) SUMO system - a key regulator in sarcomere organization. FEBS J 287: 2176-2190
- Nayak A, Wang T, Franz P, Steffen W, Chizhov I, Tsiavaliaris G, Amrute-Nayak M (2020) Single-molecule analysis reveals that regulatory light chains fine-tune skeletal myosin II function. J Biol Chem 295: 7046-7059
- Nayak A*, Lopez-Davila AJ, Kefalakes E, Holler T, Kraft T, Amrute-Nayak M (2019) Regulation of SETD7 Methyltransferase by SENP3 Is Crucial for Sarcomere Organization and Cachexia. Cell Rep 27: 2725-2736 e4
- Amrute-Nayak M, Nayak A, Steffen W, Tsiavaliaris G, Scholz T, Brenner B (2019) Transformation of the Nonprocessive Fast Skeletal Myosin II into a Processive Motor. Small 15: e1804313
- Nayak A*, Reck A, Morsczeck C, Muller S (2017) Flightless-I governs cell fate by recruiting the SUMO isopeptidase SENP3 to distinct HOX genes. Epigenetics Chromatin 10: 15
- Jung J, Nayak A, Schaeffer V, Starzetz T, Kirsch AK, Muller S, Dikic I, Mittelbronn M, Behrends C (2017) Multiplex image-based autophagy RNAi screening identifies SMCR8 as ULK1 kinase activity and gene expression regulator. Elife 6
- Nayak A, Muller S (2014) SUMO-specific proteases/isopeptidases: SENPs and beyond. Genome Biol 15: 422
- Nayak A, Viale-Bouroncle S, Morsczeck C, Muller S (2014) The SUMO-specific isopeptidase SENP3 regulates MLL1/MLL2 methyltransferase complexes and controls osteogenic differentiation. Mol Cell 55: 47-58
- Raman N, Nayak A, Muller S (2014) mTOR signaling regulates nucleolar targeting of the SUMO-specific isopeptidase SENP3. Mol Cell Biol 34: 4474-84
- Nayak A, Glockner-Pagel J, Vaeth M, Schumann JE, Buttmann M, Bopp T, Schmitt E, Serfling E, Berberich-Siebelt F (2009) Sumoylation of the transcription factor NFATc1 leads to its subnuclear relocalization and interleukin-2 repression by histone deacetylase. J Biol Chem 284: 10935-46
Collaboration
-
Dr. Chiara Luanzolo
Institute of Biomedical Technologies (ITB)-CNR, Chromatin and Nuclear architecture Laboratory, at Istituto Nazionale di Genetica Molecolare "Romeo ed Enrica Invernizzi” Milan, Italy - Prof. Riikka Kivela
Stem Cells and Metabolism Research Program, Faculty of Medicine. University of Helsinki, Finland. Faculty of Sport and Health Sciences. University of Jyväskylä, Finland
- Dr. Julien Gondin
Institut NeuroMyoGène (INMG) Physiopathologie et Génétique du Neurone et du Muscle (PGNM) UMR CNRS 5261 – INSERM U1315, Lyon, France. -
Prof. Dr. med. Michael Heuser
Department of Hematology, Hemostasis, Oncology and Stem Cell Transplantation, Hannover Medical School - Prof. Dr. Christian Bär
Institute of Molecular and Translational Therapeutic Strategies, Hannover Medical School, Germany
Teaching
- Practical courses for medical students (Human medicine and dentists)
- Seminars for medical students
- Practical courses for biology students
- Practical courses for MSc “Biomedicine” students
- Ph.D. theses in Biology and Medicine