The CI hearing prosthesis does not improve speech comprehension equally quickly and well for everyone. A research team from MHH and the University of Oldenburg is now investigating how the brain adapts to electrical hearing.
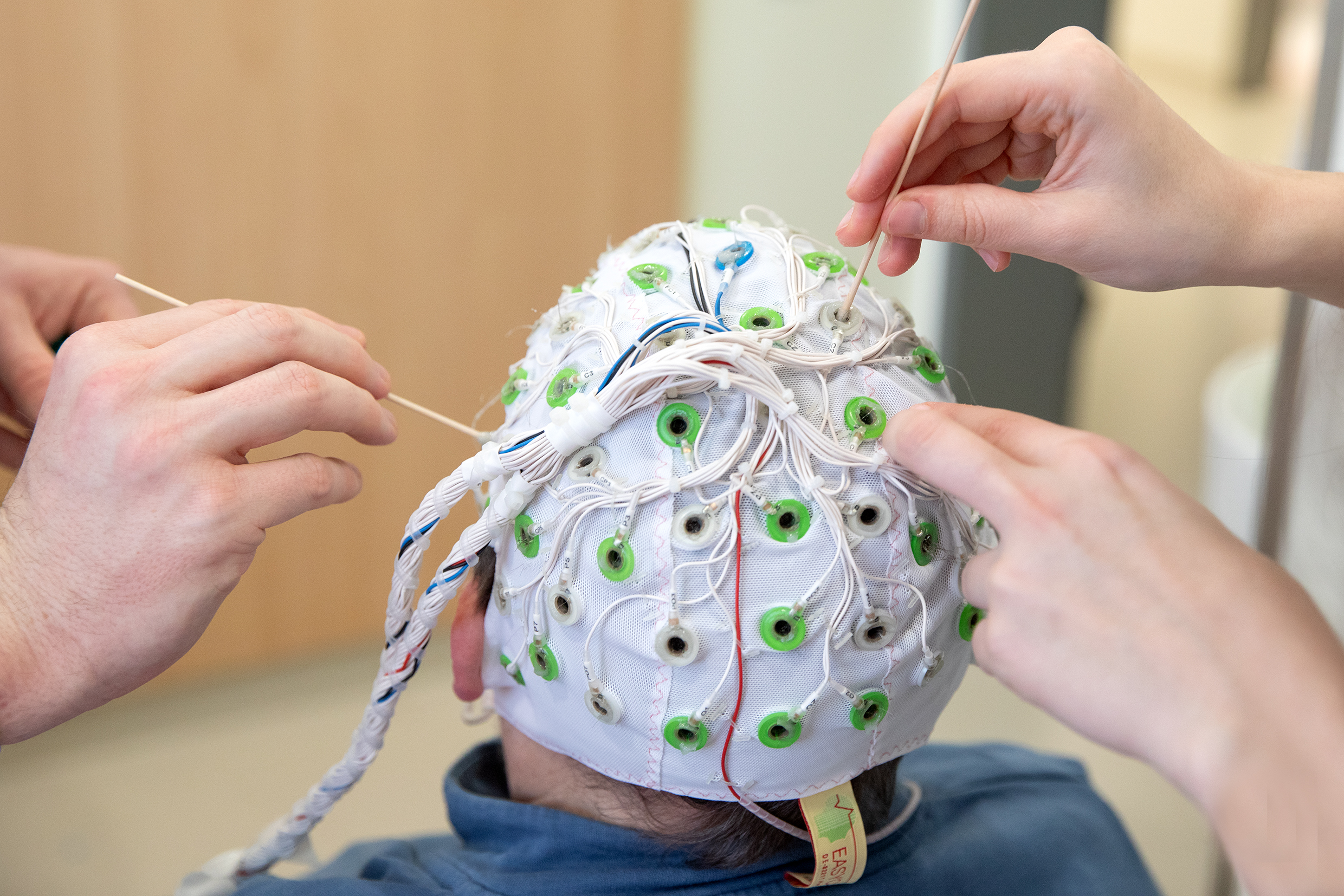
Before the examination, the electrodes of the EEG cap must be coated with contact gel. Copyright: Karin Kaiser / MHH
When hearing aids are of little or no help, so-called auditory implants are also used to treat hearing loss. The most widespread of these is the cochlear implant (CI). In Germany alone, this hearing prosthesis gives around 50,000 people who were born deaf or have become deaf in the course of their lives access to the world of hearing. The CI stimulates the auditory nerve directly via implanted electrodes in the cochlea of the inner ear. In order to interpret the new signals and perceive them as sounds, tones and speech, those affected have to train their brain to do so.
However, how quickly and how well the CI improves hearing ability varies greatly from person to person. While some people understand speech just a few hours after the CI is inserted, others need years to do so. Although it is already known that deaf people who have recently become deaf are usually the quickest to adapt to the implant, the exact mechanisms of how the brain adapts to the implant are still largely unknown. A research team from the Department of Nuclear Medicine at Hannover Medical School (MHH), together with the German Hearing Centre at MHH and the University of Oldenburg, is now seeking to clarify this as part of the Hearing4all Cluster of Excellence. The German Research Foundation (DFG) is supporting the project with additional funding totalling around half a million euros.
Differences in speech processing
The quality of care with a cochlear implant is essentially measured by the extent to which the wearer of the hearing prosthesis understands speech - especially in acoustically difficult situations with background noise or even disruptive factors such as traffic noise or multiple speakers. This requires complex auditory processing, in which brain networks also play a role. "In our study, we are comparing the speech processing of CI users with different levels of speech comprehension," says project leader Professor Dr Georg Berding, senior physician at the Department of Nuclear Medicine and head of the "Neuronuclear Medicine" working group.
One of the participants is Karin Raasch. After a total of four sudden hearing losses, she has only five per cent residual hearing. She has been wearing a cochlear implant since 2007. Karin Raasch travelled all the way from Cologne to Hanover for the test, which lasted several hours. "I'm doing this for science," she explains and smiles. Sentences are fed directly into her implant via a computer. Raasch has to decide at the touch of a button whether they make sense or not. A further test is then carried out, during which additional background noise is played.
Better image quality despite low radiation dose
The researchers use positron emission tomography (PET) and electroencephalography (EEG) to simultaneously measure how the hearing implant stimulates the test person's brain during speech processing and the underlying mechanisms. While the EEG shows the processing of the signals received via the CI precisely over time, PET enables the exact spatialisation of where this occurs in the brain. Minimal quantities of low-level radioactive substances, known as tracers, are used for this. Karin Raasch receives water via a vein access, which contains some water molecules with the radioactive oxygen isotope 15O, which was produced in MHH's own particle accelerator. With a half-life of just two minutes, this decomposes quickly, so that the patient's radiation exposure during the entire examination with several tracer doses is roughly on the same scale as an X-ray computed tomography scan.
A central aspect of the project is to reduce the tracer dose as much as possible. "To do this, we artificially reduce the raw data supplied by the PET to the amount of data we would receive with a lower tracer dose, so to speak," says Malte Voskamp, a research associate in the working group. This results in blurred images, which are then processed with the help of artificial intelligence (AI). "Denoising" is the name of the process in which the AI is to help convert the blurred PET images in such a way that they still provide reliable diagnostic information - similar to a sharper PET image with a higher tracer dose.
Previously deaf people use other regions of the brain when listening
Once the tracer enters the bloodstream, it spreads throughout the body. "With 15O water, we can therefore also visualise the blood flow in the brain," explains Professor Berding. If a brain region is particularly active, it is supplied with more blood and more tracer is present there. The researchers can then see this on a screen afterwards. Which regions are activated in detail varies slightly from patient to patient. In addition, formerly deaf people who have been fitted with a hearing prosthesis sometimes use different regions of the brain for hearing processing than people with normal hearing. On the other hand, they process visual impressions - previously during deafness - in the area of the brain that is actually responsible for acoustic signals. "Cross-modal plasticity" is what scientists call the ability of our brain to utilise brain regions that normally belong to another system when one sensory system is temporarily lost. When hearing electrically with a CI, this flexibility can have both positive and negative effects on hearing function. "The brain therefore plays a decisive role in how well a CI works," says the project manager.
Root cause research thanks to combined imaging
Until now, it has only been possible to determine how well or poorly a CI user can understand speech using precise hearing tests. The combined PET/EEG recordings, on the other hand, can be used to investigate the causes of the different auditory processing strategies used by those affected and why this results in different speech comprehension. "In future, we will be able to support the development of therapeutic strategies that specifically improve adaptation to electrical hearing," hopes Professor Berding. And this has far-reaching consequences for CI users. "Hearing loss not only significantly impairs participation in society, it also has a considerable impact on quality of life," emphasises the hearing researcher. "It is a risk factor for other agage-related disorders such as the development of depression and dementia."
Text: Kirsten Pötzke