In MS, misdirected immune cells damage the sheaths of the nerve cells in the brain. Researchers at the MHH have discovered a repair mechanism.
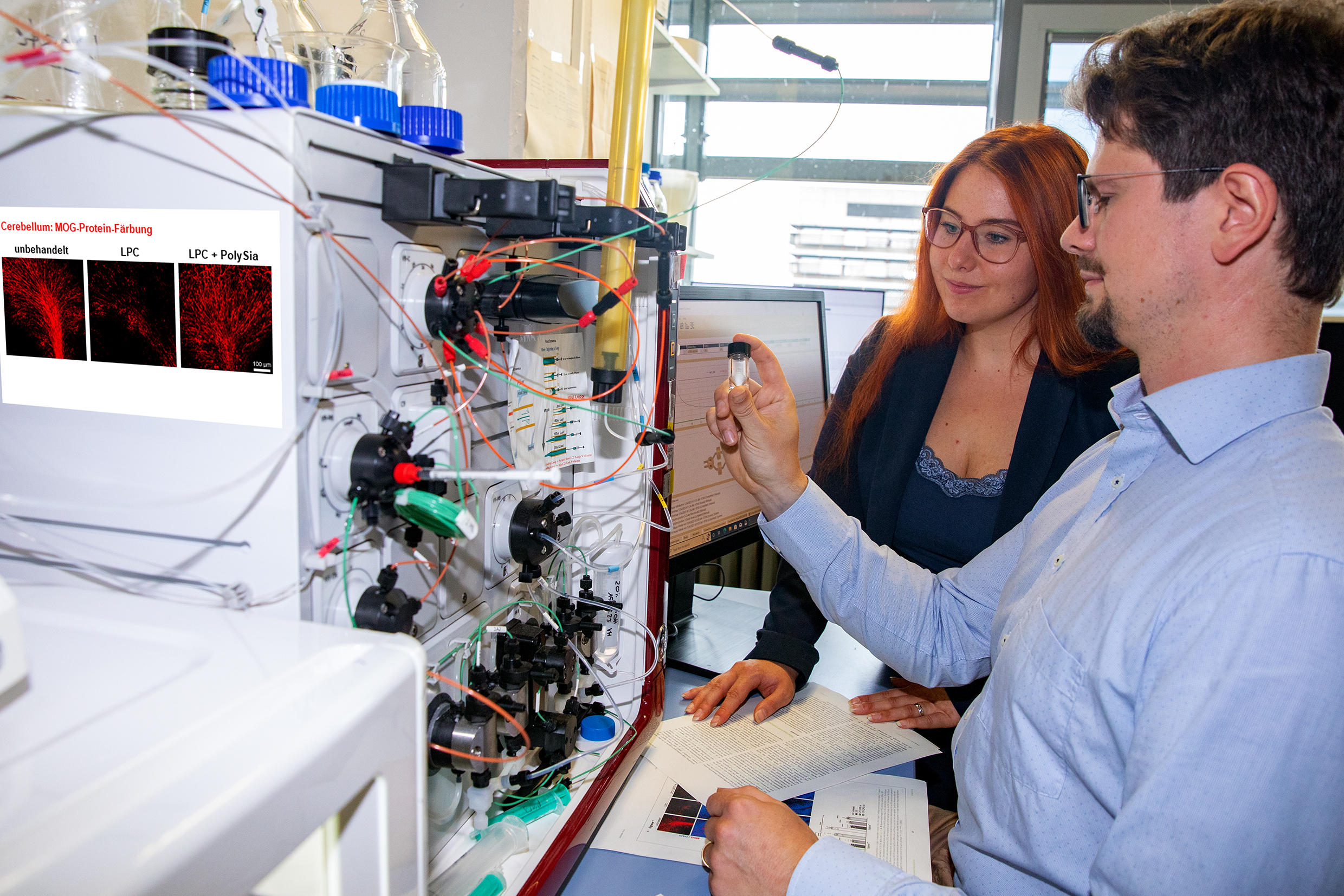
Relying on the sugar compound polysialic acid to repair damaged nerves in the brains of people with MS: Dr. Lara-Jasmin Schröder and Dr Hauke Thiesler. Copyright: Karin Kaiser / MHH
Multiple sclerosis (MS) is an inflammatory autoimmune disease of the central nervous system (CNS). In Germany, more than 280,000 people are affected. In most cases, MS progresses in relapses, which occur completely irregularly as excessive inflammatory reactions in the spinal cord and brain. In the process, misdirected immune cells destroy the protective myelin sheaths of the nerve fibres and thus damage the nerves. High-dose cortisone is usually used to slow down the inflammation. Preventive immunotherapy is also used to reduce the number and severity of attacks. It is true that the nerve fibre sheaths can be partially restored by the body's own repair processes. But this spontaneous remyelination usually proceeds incompletely in MS patients or fails to occur at all. And to date, there is no drug that promotes this repair. Researchers from the Department of Neurology with Clinical Neurophysiology and the Institute of Clinical Biochemistry at the Hannover Medical School (MHH) have now discovered a naturally occurring mechanism that can be used to decisively improve the repair of the myelin sheaths.
Sugar compound activates immune cells of the brain
The focus here is on the microglial cells of the brain. In addition to their work as "rubbish collectors" for the removal of damaged cells and foreign bodies, the microglia also take on tasks for the immune response and constantly look for signs of injury or infection. If there is a problem, the microglial cells are activated and release cytokines and other signalling molecules. This attracts other immune cells such as T and B cells, which normally reside outside the brain. The body's own sugar compound polysialic acid plays a crucial role in the activation of microglia. "The microglia has an immune receptor called Siglec-E that recognises polysialic acid," explains biochemist Dr. Hauke Thiesler. If the sugar molecule binds to the receptor, the microglia cells switch from the state "pro-inflammatory" to "anti-inflammatory". This regulatory mechanism can apparently also be controlled from outside. By externally adding polysialic acid to cultures with living tissue sections, the researchers were able to show that previously destroyed myelin sheaths were almost completely renewed as a result of an anti-inflammatory effect of polysialic acid on the microglia. The results are published in the journal Frontiers in Cellular Neuroscience.
Programming key cells for healing
"The microglial cells are the key cells that do the work directly on site and which we want to guide in a certain direction, so to speak, with the help of polysialic acid and thereby programme them for healing," says the biochemist. Because the destruction of the myelin sheaths and nerve cells has serious consequences that can affect all brain and spinal cord functions - but mainly the ability to move and coordinate, the sense of touch and the ability to see. For a large proportion of patients, multiple sclerosis brings severe disabilities. Activating the self-healing powers in the brain would be a promising support in MS therapy, which currently focuses exclusively on the immune system outside, emphasises Dr. Lara-Jasmin Schröder from the Department of Neurology with Clinical Neurophysiology. "Those affected are usually 20 to 40 years old when clinical symptoms of MS first appear," says the medical biologist. This leaves plenty of time to intervene in the regeneration between MS attacks and prevent nerve damage.
Admittedly, the studies on the tissue section cultures have only limited significance. But the researchers are optimistic based on the "striking results" that myelin regulation also works in the living organism. "The advantage is that the Siglec-E receptor in the brain actually only sits on the microglia cells and the polysialic acid can therefore intervene there in a very targeted way," explains Dr. Thiesler. And because the mechanism generally reduces inflammatory activity, the procedure could also be interesting for other neurodegenerative diseases, the biochemist suspects. Next, the research team would like to test the results in the animal model and use the MS expertise available in Lower Saxony for this. "For this, we would like intensive cooperation with other research groups and plan to submit a funding application to the Institute for Biomedical Translation (IBT) Lower Saxony so that our findings reach the bedside as quickly as possible."
The original paper „Polysialic acid promotes remyelination in cerebellar slice cultures by Siglec-E-dependent modulation of microglia polarization” can be found here.
Author: Kirsten Pötzke