MHH neuroradiologist develops international guidelines for MRI imaging
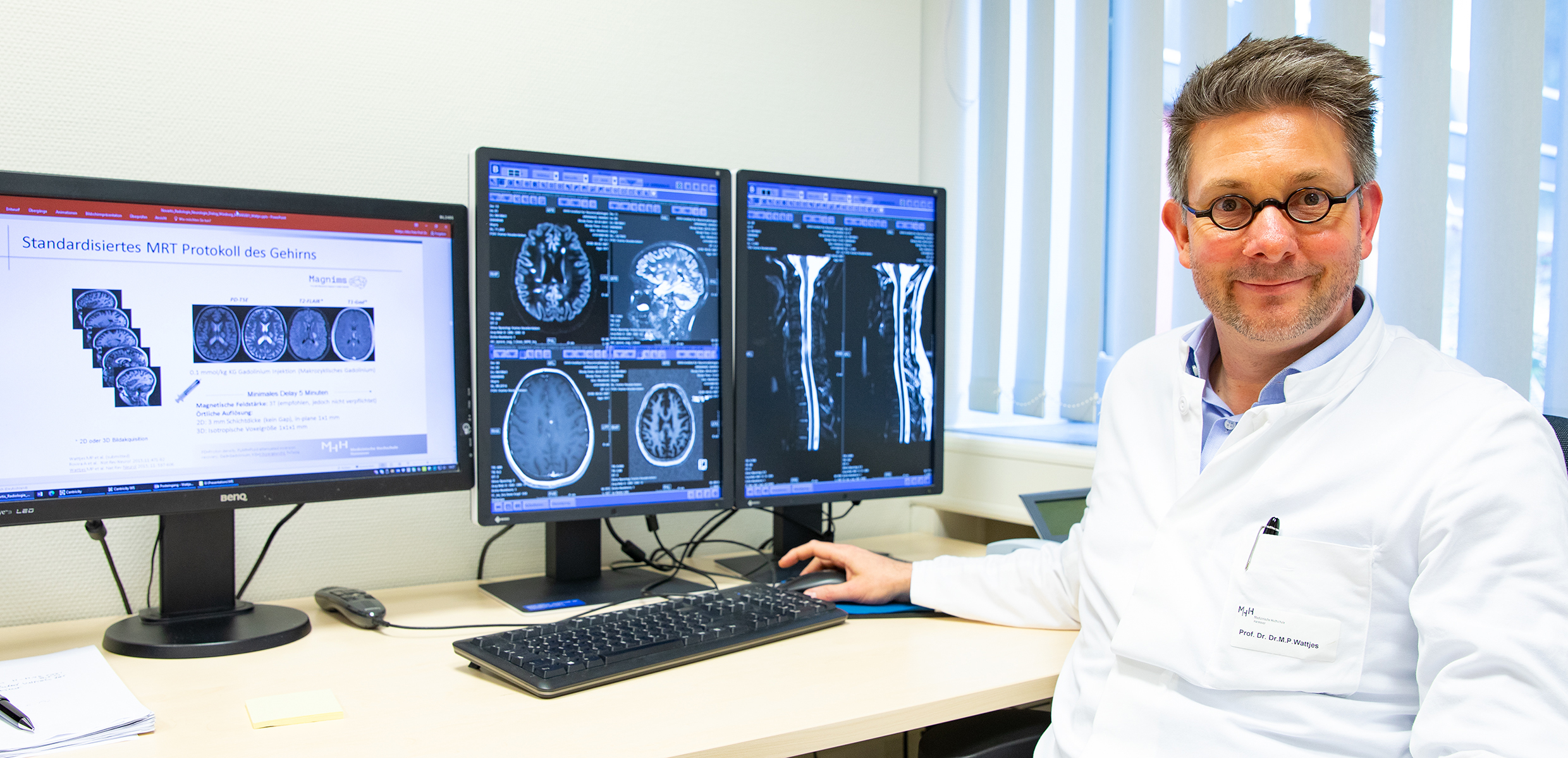
Professor Dr. Wattjes in front of two monitors with slice images of altered brain structures caused by multiple sclerosis Copyright: Karin Kaiser/MHH
Multiple sclerosis (MS) is the most common chronic inflammatory disease of the central nervous system in younger adults. According to the German Multiple Sclerosis Society, about 250,000 people in Germany suffer from MS, with more than 10,000 new cases every year. MS can be treated well, but there is no cure. Even a diagnosis can be difficult because most of the initial symptoms also correspond to those of other diseases. Magnetic resonance imaging (MRI) of the brain and spinal cord is a good method of diagnosing and monitoring MS. However, until now there have been great differences in how MRI diagnostics are actually used in the various clinics and health care systems. This is now to change. An international panel of experts led by Professor Dr. Dr. Mike P. Wattjes from the Institute for Diagnostic and Interventional Neuroradiology at the Hannover Medical School (MHH) has developed new guidelines for imaging multiple sclerosis in routine clinical practice. The recommendations are supported by both the European and North American MS organisations and have been published in the renowned journal The Lancet Neurology.
Operating guidelines for magnetic resonance imaging
"These guidelines, which are internationally standardised for the first time, are a milestone in the care of MS patients," emphasises Professor Wattjes. "Not only do they include all aspects of MS imaging, we also comment in detail on very important and current topics such as the sensible use of contrast media or the technically demanding MRI of the spinal cord." First and foremost, those affected benefit from this "instruction manual" for MRI use in MS. This is because the guideline ensures standardised patient care, giving precise recommendations on when, how and why an MRI should be performed. This concerns both the diagnosis as well as the observation of patients during therapy and the assessment of the prognosis of the course of the disease.
"The regulation is virtually the gold standard in MS imaging and is necessary for the images to be comparable at all," says the neuroradiologist. Because without mandatory standards, monitoring the course of the disease is more difficult, as it is hard to judge whether the typical tissue damage (lesions) in the brain and spinal cord have newly developed, or whether existing lesions have become larger or smaller. For the comparison of several MRI scans, it is therefore important that, for example, the spatial resolution of the images, contrast medium dose, magnetic field strength or positioning of the brain in the scanner have taken place under the same conditions.
Current research results translated into clinical practice
However, the guidelines also mean an enormous relief for the treating physicians, Professor Wattjes notes. They receive a specific application guideline for different patient groups and different stages of the disease - from children with MS to pregnant women to older patients in whom the disease no longer progresses in the typical relapses but insidiously. "Our international team has translated current research results into clinical practice and worked out exactly what makes sense for which patient at which point in time," says Professor Wattjes. The precise instructions should now enable physicians to make better diagnoses, to individually and specifically monitor the effect of drugs against MS and to make reliable prognoses on the development of the disease.
SERVICE:
For further information, please contact Professor Dr. Dr. Mike P. Wattjes, wattjes.mike@mh-hannover.de, telephone (0511) 532-2061.
You can find the original paper here .