A clinical trial under MHH leadership is testing a new therapy with immune cells against the JC virus.
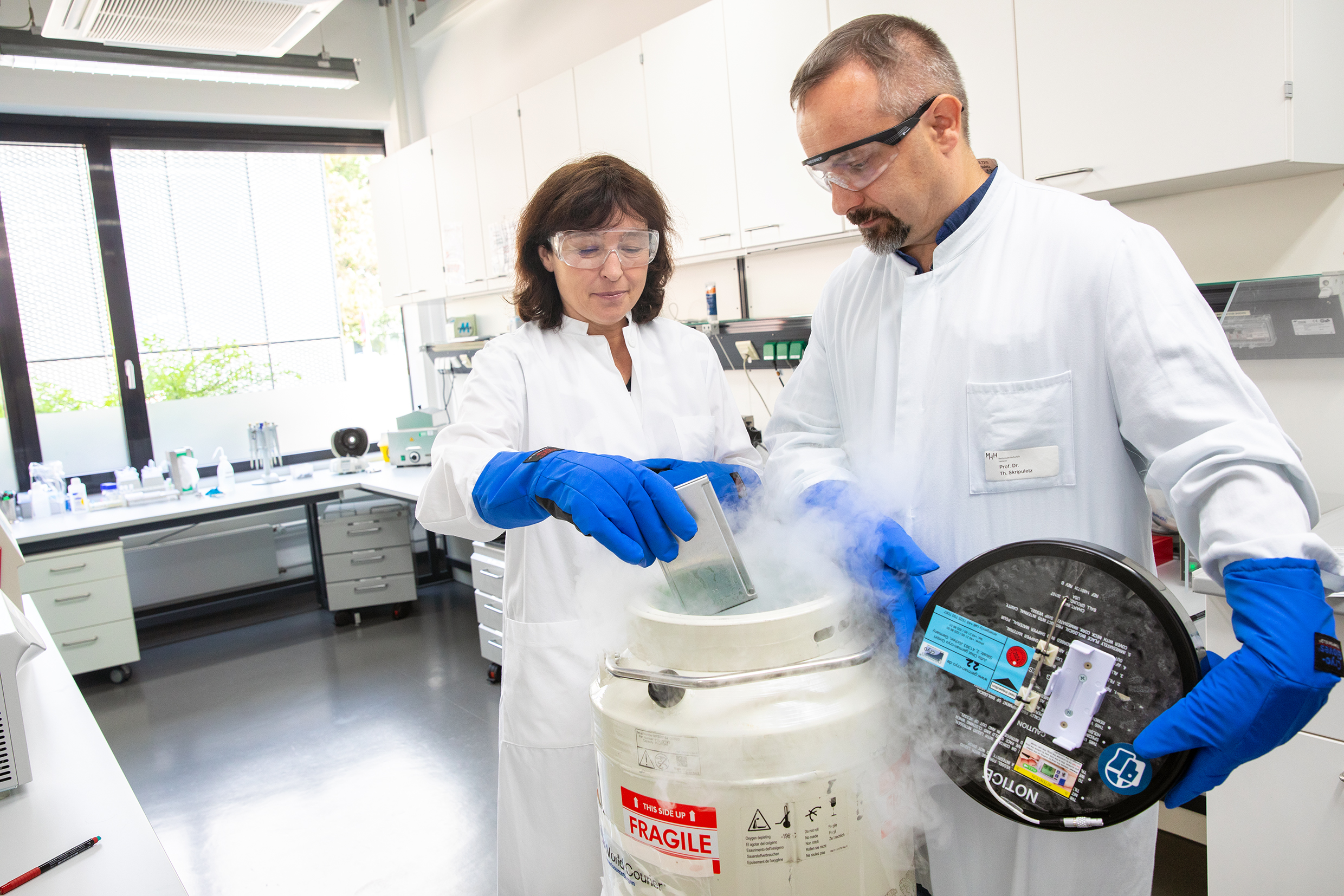
Relying on defence cells against the deadly brain infection PML: Professor Dr. Britta Eiz-Vesper and Professor Dr. Thomas Skripuletz. Copyright: Karin Kaiser / MHH
06 July 2023
Human polyomavirus 2 - formerly called John Cunningham (JC) virus - infects about 70 to 90 percent of all people worldwide without most even noticing it. But once it enters the body, the genetic material of the pathogen remains dormant there. If the immune system is weakened or shut down by a serious illness or immunosuppressive drugs, the virus is reactivated and multiplies. It can migrate into the central nervous system via the blood. Then there is a risk for progressive multifocal leukoencephalopathy (PML). This rare brain infection gradually destroys brain tissue and often leads to death within a few weeks.
But three years ago, an interdisciplinary team at Hannover Medical School (MHH) found a groundbreaking way to stop the spread of the virus. Since then, the Department of Neurology with Clinical Neurophysiology has been offering treatment with new immune cells that can push back the virus in the body of those affected. PML sufferers from Germany and abroad have since been treated at the MHH. However, these are case-by-case decisions for individual curative trials. To ensure that the therapy is available to all patients as an established method in the future, a multicenter clinical trial is to test the new therapeutic approach under standard conditions. The German Federal Ministry of Education and Research (BMBF) is supporting the project for three years with an initial 1.7 million euros.
Matched donor cells take over viral defense
Until the development of the new method, there was only one treatment option for patients taking immunosuppressive drugs: The immunosuppressants were discontinued. That way, there was a chance that PML would not develop further and possibly be cured. However, discontinuing immunosuppression is often not possible and can lead to the loss of the donor organ after a transplant, for example.
"Now, for the first time, we have an approach to combat the virus directly without major side effects," explains Professor Dr. Thomas Skripuletz, senior physician at the MHH Department of Neurology. The solution lies in the blood of healthy people who are infected with the JC virus but do not become ill. They have precisely fitting defense cells from the group of white blood cells. These T lymphocytes recognize the viral attacker as foreign to the body and initiate an immune response. When such specific T cells are transferred into the body of PML sufferers, they fight the virus there and the patient's condition stabilizes.
Unique T-cell donation registry at MHH identifies matching donors
"However, this only works without problems if the donors' cells have the same tissue characteristics as those of the recipients, i.e. are HLA-compatible," explains Professor Dr. Britta Eiz-Vesper, immunologist at the MHH Institute of Transfusion Medicine and Transplant Engineering. Because the institute is not only one of Germany's leading producer for virus-specific T cells, but also maintains the only T cell donor registry, the scientist can quickly locate suitable individuals for T cell donation. "We not only register the HLA characteristics of the blood cells in our blood donors who have consented to the registry, but also determine the number of specific T cells against different viruses at the same time," says the immunologist. In this way, effective and also compatible T cells from donors who are not related to the potential recipients can be used for cell therapy. To do this, the donor blood is processed to filter out the T cells that are being sought. Then they can either be administered directly or frozen for later use.
Viral load in neural fluid decreases
It is not only the T-cell donation registry that is unique. The speed with which the precisely matching immune cells are produced is also outstanding. "Once we have found a suitable donor, we manage production virtually overnight, which is a real survival advantage for those affected," notes Professor Eiz-Vesper. And the earlier therapy can be carried out, the lower the risk of permanent severe damage to the brain tissue. If the clinical trial now provides general proof of the treatment method's efficacy, the individual case decision could become an approved therapy for all PML patients. And that may affect more people than previously thought. "PML is probably too rarely in the focus of treating physicians, partly because there has been no cure so far," says Professor Skripuletz. In addition, he says, there are more and more immunosuppressive treatments, which favors brain infection by the virus. And in the long term, the neurologist is convinced, the therapy principle could also be extended to other neurological viral diseases.
The study was applied for together with Professor Dr Günter Höglinger. It is coordinated by the MHH Centre for Clinical Studies (ZKS) and is carried out in collaboration with MHH scientists from the Department of Neurology with Clinical Neurophysiology, the Institute for Transfusion Medicine and Transplant Engineering, the Institute for Diagnostic and Interventional Radiology, the Department of Paediatric Haematology and Oncology and the Institute for Biometry. The neurological departments of the university hospitals in Cologne, Düsseldorf, Essen, Munich and Kiel are also involved.
Text: Kirsten Pötzke