An international study led by MHH compares genomic data from national biobanks worldwide and identifies new risk factors in DNA that promote tumour development in the lining of the uterus.
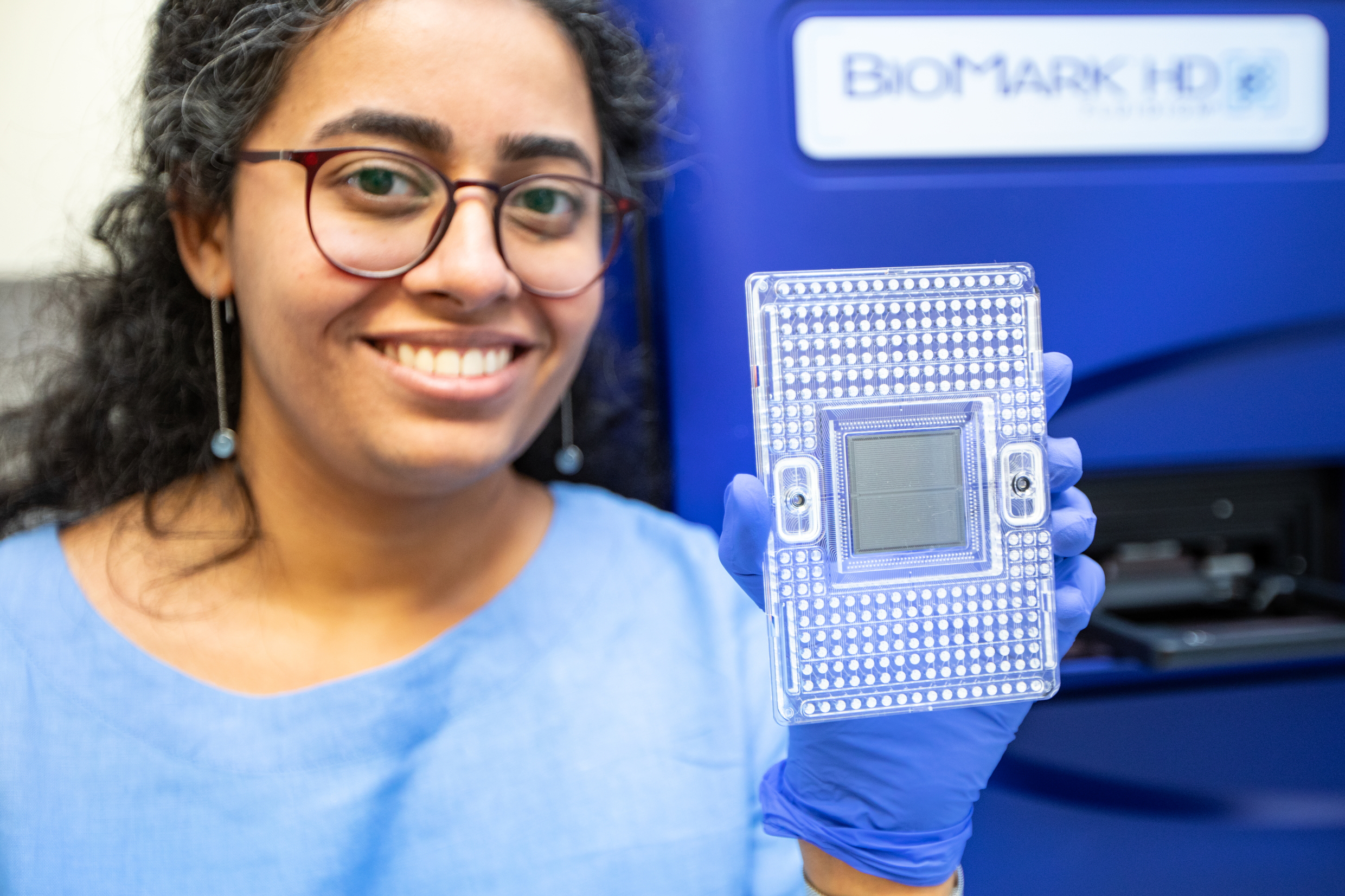
Using state-of-the-art high-throughput measurement methods, molecular biologist Dr. rer. nat. Dhanya Ramachandran examined the genetic material of patients with endometrial cancer. Copyright: Karin Kaiser/MHH
Cancer of the lining of the uterus, also known as endometrial cancer, is a common gynaecological cancer. Around 400,000 women are diagnosed with the disease every year worldwide, and around 100,000 die from it. Risk factors include obesity, diabetes and high levels of the sex hormone oestrogen. The risk of developing endometrial cancer also increases with age. Genetic predispositions, which vary widely, also play a significant role. In extreme cases, they can lead to a familial clustering of the disease and, as the basis for a hereditary syndrome, increase the risk of cancer, such as Lynch syndrome or Cowden syndrome. However, a large proportion of the genetic causes are still unclear.
Now, an international study led by the Department of Obstetrics and Gynaecology at Hannover Medical School (MHH) has discovered five new predispositions for endometrial cancer. The research team led by Dr Thilo Dörk-Bousset, head of the gynaecological research unit at MHH, collated genetic data from national biobanks in various countries and compared the occurrence of genetic changes in more than 17,000 patients with endometrial cancer with the genomes of around 290,000 healthy women. The results were then verified in further study participants from the MHH Women's Clinic. The research team discovered five new locations in the genome that are very likely to play a role in the development of endometrial cancer. The results have been published in the journal ‘eBioMedicine’.
NAV3 gene acts as a possible tumour suppressor
The researchers examined one of the new risk genes, called Navigator-3 (NAV3), in more detail in special target lines from uterine tissue. When NAV3 was deactivated, the uterine cells grew faster. Excessive NAV3 activity, on the other hand, led to cell death. ‘These results suggest that NAV3 normally limits cell growth in the endometrium and thus suppresses cancer formation as a so-called tumour suppressor gene,’ explains Dr. Dhanya Ramachandran, molecular biologist and first author of the study. ‘Accordingly, NAV3 is greatly reduced in endometrial carcinomas.’
More accurate prediction and potential new therapeutic approaches
The study increased the number of known genomic risk factors for endometrial cancer from 16 to 21. ‘This brings us one step closer to our goal of predicting the risk of hereditary uterine cancer as accurately as possible,’ says Dr Dörk-Bousset.
‘The more genes we find that are responsible, the more accurately we can calculate the probability of a woman developing endometrial cancer.’ However, this not only improves individual prediction. ‘If we understand which genes play a role in tumour development and what exactly they do, we also have potential targets for preventive strategies and new therapeutic approaches,’ says the biochemist and specialist in human genetics. The NAV3 gene appears to be a promising new candidate, and its regulation is now the subject of further investigation. ‘Today's basic research is of central importance for tomorrow's cancer therapy,’ says Professor Dr Peter Hillemanns, Director of the MHH Women's Clinic and Deputy Director of the Comprehensive Cancer Centre Lower Saxony.
The study was funded by the Wilhelm Sander Foundation. In addition to the MHH, other clinics and research institutions from Australia, Belgium, China, Germany, Great Britain, Israel, Italy, Canada, Kazakhstan, Sweden and the USA were involved.
The original paper ‘GWAS meta-analysis identifies five susceptibility loci for endometrial cancer’ can be found here.
Text: Kirsten Pötzke