Cartilage hardly regenerates due to a small number of blood vessels and nerves. We recently started a project in which we are looking for innovative solutions based on novel biomaterials and novel small molecules. We are carrying out this project together with Prof. Dorothea Brüggemann, Bremen, and Prof. Oliver Plettenburg, Hanover.
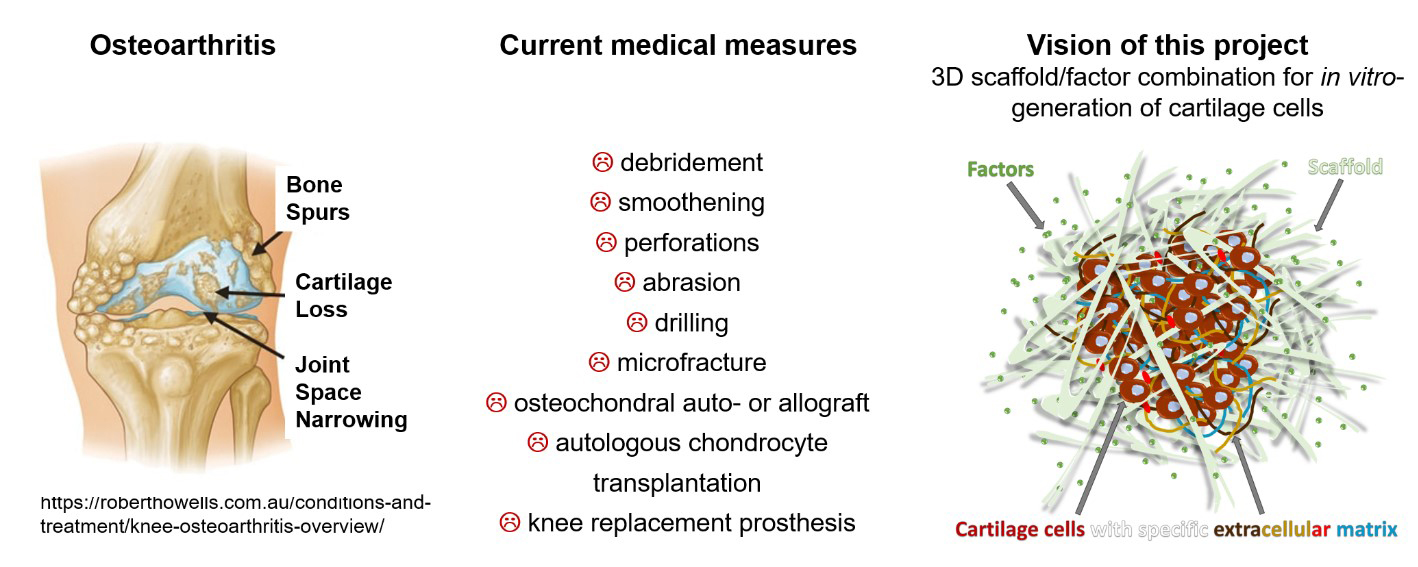
Funding since 2015
Contact person: Prof. Dr. rer. nat. Andrea Hoffmann
Current prosthetic hands based on robotic functions are still very expensive, technically far too fragile and virtually impossible to control intuitively. For these reasons, they have not yet found widespread technical application in arm prosthetics. As a rule, arm prostheses are either only cosmetic replicas of the lost limb or they only offer greatly simplified functions compared to the human hand.
In order to change this, the research project "Softpro - Synergy-based Open-source Foundations and Technologies for Prosthetics and Rehabilitation" aims to bring together and further develop available robot technologies in an open network of excellence in Europe. It is funded with € 7.4 million from the European Union's "Horizon 2020" research and innovation program.
The six pillars of the research project are sensorimotor synergies from neuroscience, human-robot interaction from robot technology, the functional simplification of everyday hand movements for their prosthetics, new strategies for assessing the progress of treatment for arm amputees, the development of shared open-source sources for bringing together the expertise of developers and users, and the close integration of research centers with clinical institutions and industry.
Funding since 2016
Contact person: Dr. Eike Jakubowitz
Homepage: http: //www.softpro.eu/

Motivation: Misalignments of the knee axis in the frontal plane lead to excessive one-sided loading of the knee and are associated with increased degeneration of the joint compartment. An efficient therapy is growth control with existing residual growth of the patient. However, this treatment often results in a rebound effect (recurrence of the deformity) after removal of the implant. The causes of this effect have not yet been sufficiently researched. As a result, there are no standardized guidelines for the optimal time for surgical removal of the implant. However, this timing is crucial for the long-term success of axial corrections. In addition, the indication for implant removal is based on static measurements during stance, which do not represent the actual loading situation and the individual compensation mechanisms during walking.Aim: The aim of the study is to investigate the influence of dynamic loading during walking on the rebound effect after surgical growth control with tension-bandage plates.Methods: Gait analysis and standing radiographs will be performed the day before implantation and explantation of the plates. To analyze the rebound effects, a non-invasive gait analysis will be performed 6 and 12 months after explantation. The daily cumulative load will be determined using an activity meter. In addition, multi-body simulations will be performed to determine the knee contact forces under the influence of the acting leg muscles and to compare these with the results from the gait analysis. Participants: 142 children with idiopathic varus or valgus leg deformities and 60 normally developed children as a control group in the same age range. Time frame: The expected duration is 3 years. Patients and the control group will be recruited within the first six quarters. The expected time to axis correction by growth guidance is on average 12 months, the follow-up after removal of the plates is 6 and 12 months.Expected results: According to the current hardware removal algorithm, which has so far been based on static measurements, not all patients will show a natural load in the knee after explantation. Since the load situation affects bone remodeling, non-physiological loading could increase the rebound effect. The results of this study may provide the first insights into the mechanical integrity of bone and muscle during and after growth control. These findings could lead to an improvement in the treatment algorithm for growth control
Funding since 2018
Contact person: Dr. Eike Jakubowitz
Patients have been treated with the so-called socket technique after an amputation for almost a century. Despite ongoing developments in prosthetics, complications can occur when wearing the prosthesis. In extreme cases, patients cannot be mobilized using the socket technique. An alternative here is osseointegrated prosthesis anchoring. An implant is inserted into the remaining femur and guided outwards through the skin at the end of the residual limb. The osseointegrated prosthesis anchoring replaces the stem and creates a direct connection between the prosthetic leg and the musculoskeletal system. Muscle volume is lost with an amputation, which leads to an imbalance in the musculature. This is often compensated for by greater use of the contralateral side, which promotes degenerative changes in the joints. A significant correlation between amputation and an increased risk of gonarthrosis of the contralateral leg has been demonstrated.
Based on our own preliminary work, a patient-specific multi-body model of the musculoskeletal system of transfemoral amputees is being developed. The various fitting concepts, such as the socket technique and osseointegrated prosthesis anchoring, are to be taken into account. In addition, the model includes the special muscle and bone situation and is intended to determine the muscle forces during everyday activities, such as walking on level ground and climbing stairs, as well as the contact force. The use of imaging, gait analysis and multi-body simulation is planned.
The aim of the project is to investigate the effect of an osseointegrated prosthetic fitting compared to conventional fittings on gait pattern and joint loading. Two working hypotheses are to be tested:
1a) Compared to healthy subjects, the patients with a socket fitting show a gait pattern that leads to increased loading in the contralateral hip joint.
1b) Patients with an osseointegrated prosthesis anchorage show a gait pattern that leads to increased stress in the contralateral hip joint compared to healthy subjects.
2) Patients who are fitted with an osseointegrated prosthesis anchorage have a more symmetrical gait pattern than patients who are fitted with the conventional socket technique and have a lower load in the hip joint.
In addition, procedures for residual limb design are to be scrutinized and optimized with the clinical partner. As a result, a femoral stump model is to be developed that features optimized muscle attachments to reduce energy expenditure. In the long term, this could improve and maintain the quality of life of affected patients, for example by clarifying the development of osteoarthritis caused by increased stress on the contralateral hip joint.
Funding since 2017
Contact person: Dr. Bastian Welke
As part of this new DFG proposal, the mechanisms and functions of individual joint structures of the knee in relation to soft tissue balancing are to be investigated using in-vitro experiments and supplemented with the aid of computer simulations. Based on existing data on stability, stiffness and soft tissue inhibition of individual structures of the knee joint from the current literature, an optimal, systematic sequence of soft tissue release will be developed and objective target parameters of soft tissue balancing will be determined. The findings from the literature are to be supplemented by structured tissue resection experiments on the knee specimen followed by stiffness tests on the robot. The information gathered from the literature and the experiments will also be used as a basis for the development of a comprehensive musculoskeletal multibody model of the knee, which can be used to project further approaches to soft tissue balancing within the project. This project lays the foundation for a model-based, patient-specific simulation of soft-tissue balancing from which a planning tool for knee TEP can be developed in subsequent projects. This can then support the surgeon with suggestions regarding soft tissue release during surgical planning with the help of automated multi-body simulations and thus contribute to the objectification of soft tissue balancing.
Funding since 2015
Contact: Dipl.-Ing. Dennis Nebel
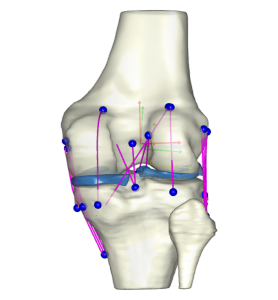
As part of this new DFG proposal, the mechanisms and functions of individual joint structures of the knee in relation to soft tissue balancing are to be investigated using in-vitro experiments and supplemented with the aid of computer simulations. Based on existing data on stability, stiffness and soft tissue inhibition of individual structures of the knee joint from the current literature, an optimal, systematic sequence of soft tissue release will be developed and objective target parameters of soft tissue balancing will be determined. The findings from the literature are to be supplemented by structured tissue resection experiments on the knee specimen followed by stiffness tests on the robot. The information gathered from the literature and the experiments will also be used as a basis for the development of a comprehensive musculoskeletal multibody model of the knee, which can be used to project further approaches to soft tissue balancing within the project. This project lays the foundation for a model-based, patient-specific simulation of soft-tissue balancing from which a planning tool for knee TEP can be developed in subsequent projects. This can then support the surgeon with suggestions regarding soft tissue release during surgical planning with the help of automated multi-body simulations and thus contribute to the objectification of soft tissue balancing.
Funding since 2015
Contact: Dipl.-Ing. Dennis Nebel
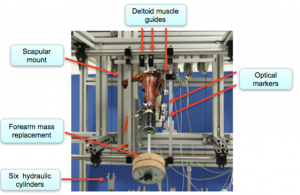
The implantation of an inverse shoulder joint prosthesis (ISP) has been established as an effective surgical procedure for improving active shoulder joint mobility and reducing pain in patients with a defective arthropathy. However, postoperative dislocation of the prosthesis occurs in a significant proportion of patients due to the deficient muscular stabilizers. The cause of instability of the shoulder or an insufficient range of motion after implantation of an ISP can potentially be attributed to the alignment of the prosthesis components as well as to the patient's underlying pathology, a chronic rotator cuff defect, which is not resolved by the implantation. A key problem in the medical treatment of patients with an ISP in the case of a residual rotator cuff is the lack of information regarding the risk of instability after treatment, which depends on the damage pattern. Although surgical treatment of patients with an ISP provides good results compared to treatment with an anatomical shoulder prosthesis, the surgeon still lacks information on optimal soft tissue management in the treatment of patients with a deficient rotator cuff in order to achieve maximum stability and range of motion. The two main objectives of the present research project are therefore,
1. to biomechanically investigate the role of inter-articular soft tissue tension and in particular the effect of individual musculo-tendinous stabilizers on shoulder stability before and after implantation of an inverse shoulder joint prosthesis.
2. to determine the optimal soft tissue management depending on the patient-individual damage pattern of the musculo-tendinous stabilizers in order to achieve optimal stability of the joint and maximum range of motion after prosthetic treatment.
Funding since 2016
Contact person: Dipl.-Ing. Dennis Nebel