Background
The Research Group Molecular Psychiatry is mainly focused on neuroepigenetics.
Epigenetic mechanisms serve to regulate transcriptional activity and are partly hereditary. Through DNA methylation and post-translational modification of histone proteins, the structure of DNA can be altered (chromatin remodeling) in such a way that individual genes are switched on and off in a spatio–temporal manner. Short RNA species and posttranscriptional RNA modifications (RNA editing; alternative splicing) are further substrates of epigenetic processes. Environmental cues (stress, diet, substance abuse and adverse life experiences) mediate their effect on cellular pathways via epigenetics.
Therefore, the special importance of epigenetic processes in psychiatry has been demonstrated both in disease development, maintenance and cure of mental illness, and in the biological coding of disease susceptibility (vulnerability) or insusceptibility (resilience). Epigenetic processes are also of particular interest for the longitudinal transmission of mental illness over generations.
To investigate these phenomena, we use an entire spectrum of molecular biological methods, which are provided by the Laboratory of Molecular Neuroscience. We systematically design and execute clinical studies followed by validation in cell culture and animal models towards our mission statement of translational research.
Within the Department of Psychiatry, Social Psychiatry and Psychotherapy there is close cooperation with the research groups
- Alcohol, Nicotine and Drug Addiction
- Psychokardiology and Psychotherapy
- Difficult to Treat Depression / Non-invasive brain stimulation
- Clinical psychology and Sexual Medicine
Aim of the research group
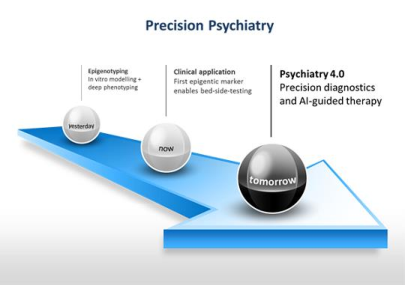
One of the main obstacles in today's psychiatric research is the apparent discrepancy between the diagnostic criterias, mainly coined at the end of the 19th century, and modern neurobiological concepts of normal and impaired brain function, which leads to a delay in the development of new and more effective therapies.
One approach to bridge this gap is offered by "personalized" or "precision" psychiatry, which will identify more homogeneous subgroups of mentally ill patients on the basis of a bio-psychosocial disease model and will provide these specific therapies. In this context, a major research goal of our research group is the use of epigenetic markers to identify and categorize biologically different subgroups of psychiatric disorders, using response to specific therapies as a primary phenotype. Once a potential marker is discovered, we not only focus on rigorous replication in clinical cohorts, but also try to understand how specific regulation of a particular gene leads to (non) response to specific therapies. To answer these questions, we use animal and cell culture models as well as patient samples including induced pluripotent stem cells (iPSC) and post mortem brain tissue, and employ a broad spectrum of state-of-the-art molecular testing methods.
Reterospectively, Our molecular findings are complemented with functional imaging, psychopathological, test-psychological and other clinical data of the patients*, because even the best molecular analyses of psychiatric disorders need to be informed by the clinic and should be transferable back to the clinic afterwards. To enable this flow, large cohorts of patients with excellent and multimodal phenotyping are needed. One way to recruit these cohorts is to establish a broad-content system that allows the use of all routinely collected clinical data. By establishing a data warehouse system, all data from the clinical information systems can be used for specific research questions. We have supplemented this system with large patient registries for special indications (for example, a registry for the special outpatient clinic that treats patients with Prader-Willi syndrome and psychiatric disorders), therapies (Lower Saxony EKT-Outcome Registry - NEKTOR) or side effects (AMSP; pharmacovigilance in gerontopsychiatry) and expanded it to include biobanking of blood and other samples according to strict pre-analytical protocols. In order to achieve a high quality of phenotypic data, we have implemented standardized diagnosis and treatment algorithms. These algorithms can be easily adapted to incorporate new findings (e.g. potential new biomarkers guiding treatment). At the same time, large patient* collectives open up the possibility to understand new findings from basic research, such as structural variations of the genome in people suffering from psychosis, and to better understand and clinically exploit them through multimodal reverse phenotyping.
Large amounts of data from different areas of basic research (-omics, imaging) or clinical research contain a wealth of information. In addition, new developments in sensor technology (e.g. through wearables) or app-based examinations, as well as the possibility of using all the clinical data from routine care, facilitates an extensive amount of data that can no longer be handled with classical evaluation methods of inferential statistics. To access this information, new methods of data analysis such as pattern recognition based on artificial intelligence / neural networks are necessary.
In recent years we have gained experience in the use of these "big-data" methods for the integrative analysis of molecular and clinical data. The use of self-learning algorithms not only helps to discover new and unexpected relationships between molecular and clinical data, but also promotes the development of diagnosis and treatment algorithms in an iterative and evolutionary way (Plan-Do-Check-Act (PDCA) cycle to integrate patient care and research goals), thus paving the way for more precise psychiatry.
Establishment of DNA methylation markers in patients suffering from therapy-resistant depression
We were able to identify DNA methylation markers indicating an increased risk of non-response to standard monoaminergic antidepressants (EU and US patent granted) or non-response under electroconvulsive therapy (ECT). Other DNA methylation markers that predict a positive response to ECT or specific psychotherapy treatments are currently being tested.
Selected publications:
- Lieb, K., Dreimüller, N., Wagner, S., Schlicht, K., Falter, T., Neyazi, A., Müller-Engling, L., Bleich, S., Tadić, A., & Frieling, H. (2018). BDNF Plasma Levels and BDNF Exon IV Promoter Methylation as Predictors for Antidepressant Treatment Response. Frontiers in psychiatry, 9, 511. DOI
- Moschny, N., Zindler, T., Jahn, K., Dorda, M., Davenport, C. F., Wiehlmann, L., Maier, H. B., Eberle, F., Bleich, S., Neyazi, A., & Frieling, H. (2020). Novel candidate genes for ECT response prediction-a pilot study analyzing the DNA methylome of depressed patients receiving electroconvulsive therapy. Clinical epigenetics, 12(1), 114. DOI
To extract free DNA from CSF of patients suffering from schizophrenic psychosis, a method has been established to extract small amounts of DNA from larger volumes of cerebrospinal fluid. This DNA is currently being investigated for potential changes in the methlylation patterns in the promoter region of relevant target genes.
Prader-Willi syndrome (PWS) is a rare genetic disorder. People with PWS suffer significantly more frequently from mental illnesses, especially psychoses, than the so-called "normal population". Within the framework of several research projects, a register is being established and the molecular biological causes of the development of mental illness in PWS are being researched. Furthermore, clinical questions, e.g. the establishment of new therapy options, are being investigated.
Regardless of the important evolutionary functions of nociception, cellular dysregulation can lead to hypersensitivity of pain sensation. In order to uncover the underlying regulatory mechanisms, analyses of promoter methylation of genes involved in nociception are performed in volunteers with different pain sensitivity, and different molecular biological methods are applied to analyze expression and promoter activity.
Selected publications:
- Gombert S, Rhein M, Eberhardt M, Münster T, Bleich S, Leffler A, Frieling H. Epigenetic divergence in the TRPA1 promoter correlates with pressure pain thresholds in healthy individuals. Pain. 2017 Apr;158(4):698-704. PMID: 28030472. DOI
- Achenbach J, Rhein M, Gombert S, Meyer-Bockenkamp F, Buhck M, Eberhardt M, Leffler A, Frieling H, Karst M. Childhood traumatization is associated with differences in TRPA1 promoter methylation in female patients with multisomatoform disorder with pain as the leading bodily symptom. Clin Epigenetics. 2019 Aug 28;11(1):126. PMID: 31455424; PMCID: PMC6712620. DOI
- Gombert S, Rhein M, Winterpacht A, Münster T, Hillemacher T, Leffler A, Frieling H. Transient receptor potential ankyrin 1 promoter methylation and peripheral pain sensitivity in Crohn's disease. Clin Epigenetics. 2019 Dec 31;12(1):1. PMID: 31892361; PMCID: PMC6938615. DOI
Scientific cooperations
In addition to the above-mentioned internal collaborations, we cooperate with numerous other research groups within the framework of national and international research networks (e.g., regarding eating disorders [BMBF-EDNET], borderline personality disorders, psychopharmacological effects [BMBF-NeSSy], and traumatization):
- Institute for Human Genetics
- Institute for Clinical Biochemistry
- Institute of Virology
- Clinic for Ophthalmology
- Clinic for Anaesthesiology
- Clinic for ear, nose and throat medicine
- Department of Neurology with clinical neurophysiology
- Clinic for Neurosurgery
- LEBAO
- Research Network on Eating Disorders (BMBF-EDNET)
- Research collaborations on borderline personality disorder and psychotropic drug effects (BMBF-NeSSy)
- Research Network on the Neurobiological Foundations of Pedophilia and Sexual Abuse Behavior against Children (BMBF-NeMUP)
- Centre Paul Broca, Paris
- INSERM (Centre Hospitalier Sainte Anne), Paris
Research group members
Research group leader
Prof. Dr. med. Helge Frieling
Deputy director & Founding member and scientific advisory board of the Research Core Unit Genomics of the MHH
Phone: +49 511 532 7275
Fax: +49 511 532 7276
Phone: +49 511 532 7275
Fax: +49 511 532 7276
buchholz.vanessa@mh-hannover.de
Research focus: Epigenetic analyses using Sanger
Publications: Pubmed
Phone: +49 511 532 7275
Fax: +49 511 532 7276
burkert.alexandra@mh-hannover.de
Research focus:
- Methylation-specific probe-based qPCR
- Epigenetic analyses using Sanger/Nanopore sequencing
Publications: Pubmed
Phone: +49 511 532 3167
Fax: +49 511 532 3168
deest.maximilian@mh-hannover.de
Research focus:
- Neurodevelopmental Disorders
- Prader-Willi syndrome
- Autism spectrum disorder
Excellence: Clinician Scientist in the DFG-funded program PRACTIS at the MHH
Publication: Pubmed
Phone: +49 511 532 3167
Fax: +49 511 532 3168
eberlein.christian@mh-hannover.de
Research focus:
- Research into the neurobiological basis of the development of mental illness in people with Prader-Willi syndrome.
- Care research, clinical research (type, frequency and symptoms of mental illness) and research into new drug therapy options for mental illness in people with Prader-Willi syndrome.
- Health services research, clinical research on mental illness in rare syndromal diseases (type, frequency, symptoms) and research into drug and non-drug treatment options.
Publications: Pubmed
Phone: +49 511 532 7245
Fax: +49 511 532 7276
Research focus:
- Epigenetic analyses using Sanger sequencing
- Studies of promoter activity by luciferase reporter assay
- Expression analysis via RT-qPCR and Western blot
Title of doctoral dissertation: Epigenetic regulation of the ion channel TRPA1 in the context of pressure pain sensitivity
Publications: Pubmed
Phone: +49 511 532 9191
Fax: +49 511 532 18523
Research focus:
- Media and gaming dependency
- Adverse drug reactions /UAW) in gerontopsychiatry
- Drug interactions in gerontopsychiatry
Publications: Pubmed
Phone: +49 511 532 7275
Fax: +49 511 532 7276
Research focus:
Diseases
- Schizophrenia (Biomarker CSF)
- Sexual Deviations/Paraphilia
- Depression
Methods
- Epigenetic analyses using Sanger/NGS/Nanopore sequencing
- Neural in-vitro models for visualization of synapse formation
- Patch Clamp, Calcium Imaging
Publications: Pubmed
Phone: +49 511 532 7275
Fax: +49 511 532 7276
Research focus:
- Epigenetic regulation of BDNFIV upon antidepressant treatment
- Establishment of Gene panel for therapy response for antidepressant treatment
- Effect of antidepressants on BDNF secretion by neurons and reuptake by astrocytes
- Studying chromatin composition of GDNF promoter to study its role in therapy response during MDD
Publications: Pubmed/Pathak_Hansi & PMID21734725 & PIMD28887651
Co-head of the research group "Alcohol, nicotine and drug addiction"
Phone: +49 511 532 7245
Fax: +49 511 532 7276
Excellence:
- Protein Biochemistry
- Epigenetic analysis methods
- Research on alcohol addiction and other substance drugs
- Regulation of genes in blood and brain
Publications: Pubmed