What is AAPV?
General outpatient palliative care (AAPV) looks after patients in their own homes who are suffering from an incurable, advanced illness and whose problems and complaints require regular nursing, medical and psychosocial care. Communications about the individual needs of patients and their relatives are the main focus. Alleviating symptoms and improving quality of life are the central goals of care.
The key role of GPs
As primary care providers, GPs play a key role in AAPV. As part of their professional self-image, they often see it as their responsibility, but also as their wish, to accompany their patients throughout the entire course of their illness until the end of their lives. Patients and relatives also want this continuity of care from the GP, as they have built up a close relationship of trust over years or even decades.

Background
Since around 90% of all people could be cared for at home at the end of their lives, the importance and central position of GPs is very clear. With the Act to Strengthen Hospice and Palliative Care (HPG) in 2015, palliative care by GPs was even enshrined in law. However, scientific studies have shown that integrating palliative care into the daily routine of GPs is a challenge. There is therefore a need for more in-depth research into how the implementation of GP palliative care can be facilitated.

Aims
The overarching aim of the junior research group "General outpatient palliative care in general practice" (ALLPRAX) is to improve the framework conditions for the implementation of AAPV by general practitioners in private practice. In the long term, the results of the project should help to improve AAPV for patients at the end of life.
The sub-goals of ALLPRAX are
- the systematic recording and evaluation of factors that hinder and promote AAPV in GP practices
- the development of a practical concept for the integration of AAPV into daily practice and
- the introduction and testing of the concept in terms of practical manageability and concrete effects on patient care
Publications
-
Bilgin ES, Ülgüt R, Schneider N, Stiel S. Improving primary palliative care - a Delphi consensus study on measures for general practice in Germany. BMC Primary Care. 2022; 23: 12 (PubMed)
- Ewertowski H, Hesse AK, Schneider N, Stiel S. General palliative care in general practice: development of strategies to improve structural, legal and financial framework conditions. Z Evidenz Fortbild Qual Gesundheitswes 2020; 149: 32-39. (PubMed)
- Ewertowski H, Tetzlaff F, Krause O, Eylers V, Schneider N, Stiel S. "It is one of my most important tasks that I really accompany them to the end" - A multi-perspective qualitative study on outpatient palliative care. Z Allg Med 2019, 95(4): 169-74. (Z Allg Med)
- Ewertowski H, Tetzlaff F, Stiel S, Schneider N, Jünger S. Primary palliative Care in General Practice - study protocol of a three-stage mixed-methods organizational health services research study. BMC Palliative Care 2018, 17: 21 (PubMed)
-
Grütering L, Zimansky M, Schneider N, Stiel S. Improving general outpatient palliative care in general practices - evaluation of the ALLPRAX intervention study. Z Palliativmed 2021; 22(6): 316-324 (Z Palliativmed)
- Stiel S, Ewertowski H, Krause O, Schneider N. What do positive and negative experiences of patients, relatives, general practitioners, medical assistants, and nurses tell us about barriers and supporting factors in outpatient palliative care? A critical incident interview study. GMS Ger Med Sci 2020, 18: Doc08 (PubMed)
- Stiel S, Krause O, Berndt CS, Ewertowski H, Müller-Mundt G, Schneider N. Caring for frail older patients in the last phase of life: Challenges for general practitioners in the integration of geriatric and palliative care. Z Gerontol Geriatr 2019, 53(8): 763-769 (PubMed)
- Ülgüt R, Stiel S. You can't do without a family physician. Supporting people at the end of life at home. Hospice Journal 2021, 2:33-37.
- Willinger A, Hemmerling M, Stahmeyer JT, Schneider N, Stiel S. The frequency and time point of outpatient palliative care integration for people before death: an analysis of health insurance data in Lower Saxony, Germany. J Public Health 2021, DOI: 10.1007/s10389-021-01672-1. (J Public Health)
- Zimansky M, Gerdes A, Schneider N, Stiel S. Measures to improve general outpatient palliative care from the perspective of GP practice teams. Z Palliativmed 2021, 22: 41-46 (Z Palliativmed).
-
Zimansky M, Hofmann B, Schneider N, Stiel S. Implications for health services research in GP practices using the example of an intervention study on palliative care. Z Evidenz Fortbild Qual Gesundheitswes. 2021; DOI: 10.1016/j.zefq.2021.05.001 (Z Evidenz Fortbild Qual Gesundheitswes)
News
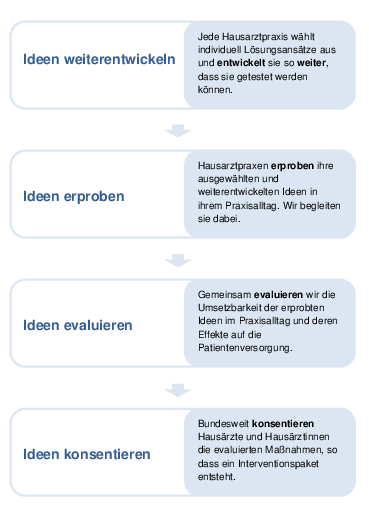
Ideas for GP practices tested and evaluated
Last year, seven GP practice teams took part in the implementation and testing of measures that can make it easier for GPs and their practice teams to provide outpatient palliative care.
We would like to thank all participants, with whose support 35 practice-related intervention measures for the further development of outpatient palliative care could be successfully tested and evaluated with regard to their relevance and feasibility.
Tested and evaluated ideas consented nationwide
The tested and evaluated intervention measures were consented nationwide for a strategy for the further development of palliative care by GPs.
A total of 20 recommendations were included in an intervention package.
The intervention measures can be assigned to the five main topics of anticipatory care for patients (I), counselling for patients and relatives (II), organization in the GP practice (III), further education and training (IV) and cooperation with other medical service providers (V).
The tested, evaluated and nationally agreed intervention package is available to download here free of charge. You can use the materials for your practice, adapt them individually and develop them further as required.
Promotion
ALLPRAX is funded as part of the BMBF's action plan for health services research (funding code 01GY1610) within the framework of the measure "Structural development in health services research" in the funding module "Junior research groups for health services research".
ALLPRAX - Contact
Prof. Dr. Dr. Stephanie Stiel (Project Manager)
Phone: +49 511 532-4548
Address
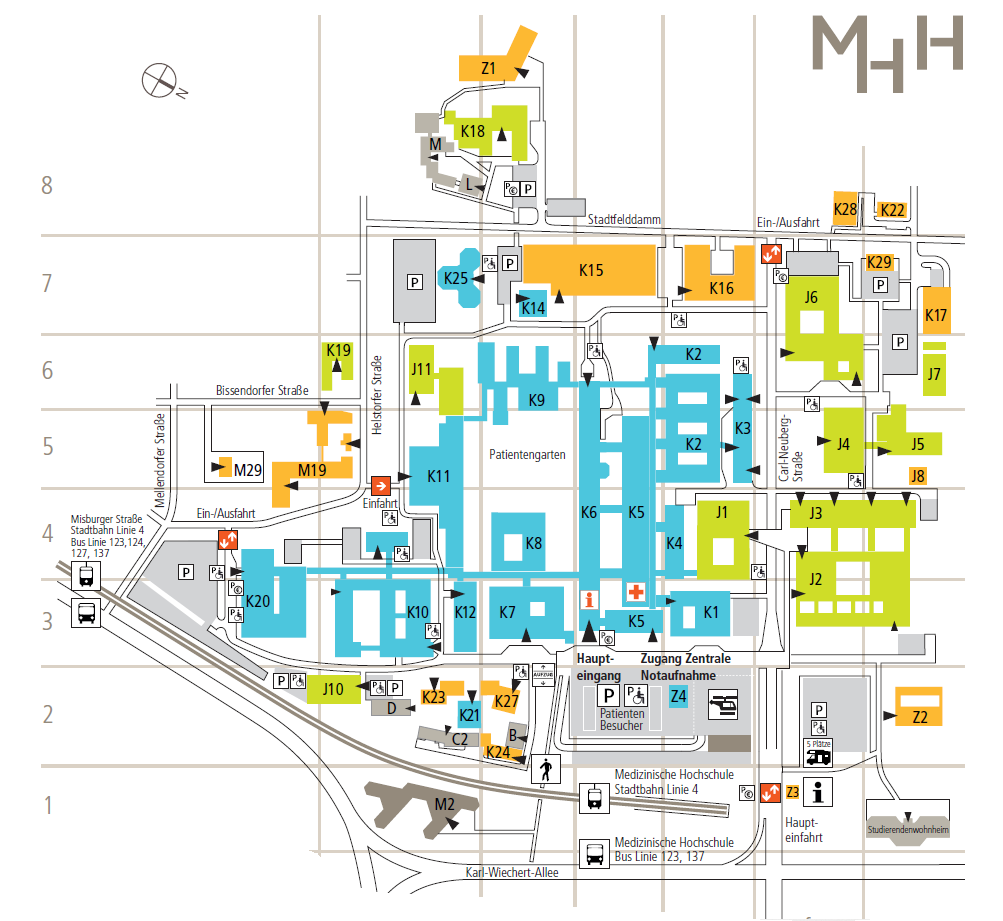
Hannover Medical School
Institute ofGeneral Medicine and Palliative Medicine
Carl-Neuberg-Straße 1
30625 Hanover