OPAL
Optimal care at the end of life

Background
Around 900,000 people die in Germany every year. Up to 90% of all people at the end of life require some form of palliative care, the vast majority of whom can be adequately cared for and supported by GPs as part of general outpatient palliative care.
General outpatient palliative care still poses considerable challenges for GPs in Germany, particularly with regard to the systematic implementation of palliative care measures. One major obstacle is the early identification of patients who could benefit from palliative care. This is made even more difficult in the case of chronic progressive diseases and multimorbidity in the last phase of life.
To this end, the German version of the Supportive and Palliative Care Indicators Tool (SPICT-DETM) was introduced, tested and evaluated as a practical decision-making aid in GP care practice. This intervention was flanked by measures at the level of two health regions in Lower Saxony.
Objectives
The overarching aim of the OPAL project was to improve the care of patients with chronic progressive diseases in the last phase of life and their relatives. The focus here was on GP care. The following were also investigated
- the use and improvement of the acceptance of SPICT-DETM by GPs
- strengthening the awareness and sensitivity of GPs for palliative situations and the targeted identification of patients who could benefit from palliative care
- an assessment of the effectiveness of action and the practical consequences for GP practice, accompanied by a strengthening of the options for action in GP care and at its interfaces.
If successful, SPICT-DETM can be used in other regions and for all groups of patients with chronic progressive diseases and improve care.

Methods
The OPAL research project was an intervention study in a pre-post design. Both qualitative and quantitative methods of health services research were used in the individual phases of the project (mixed methods design). The research project ran for a total of 42 months and was divided into three main phases:
Phase 1 - Exploration of healthcare practice:
- Expert interviews with key people in the healthcare region
- Standardized survey of general practitioners
- Interviews with relatives of deceased patients
- Analysis of routine clinical data from GP practices
- Secondary analysis of health insurance data
Phase 2 - Intervention at two levels:
- at the level of GP practices, training on and actual use of SPICT-DETM and monitoring of practices was carried out
- At the level of the health regions, health dialogues were held with stakeholders at the interfaces to GP care to provide information about the intervention in GP practices and to initiate and promote cross-sectoral cooperation
Phase 3 - Evaluation:
- As part of the process evaluation, factors promoting and hindering implementation were summarized from monitoring protocols, health dialogues and interviews with professional stakeholders and relatives
- the results evaluation consisted of a new survey of the data collected in phase 1 (t0) at t1 (pre-post comparison)
Results
The following brochure with recommendations for action was developed on the basis of the empirical data from OPAL. The recommendations for action take particular account of the perspective of GPs in end-of-life care. The experiences and wishes of experts at the interfaces to GP care and relatives were also taken into account during the development process.
Brochure "Recommendations for the care of people at the end of life and their relatives"
Cooperation
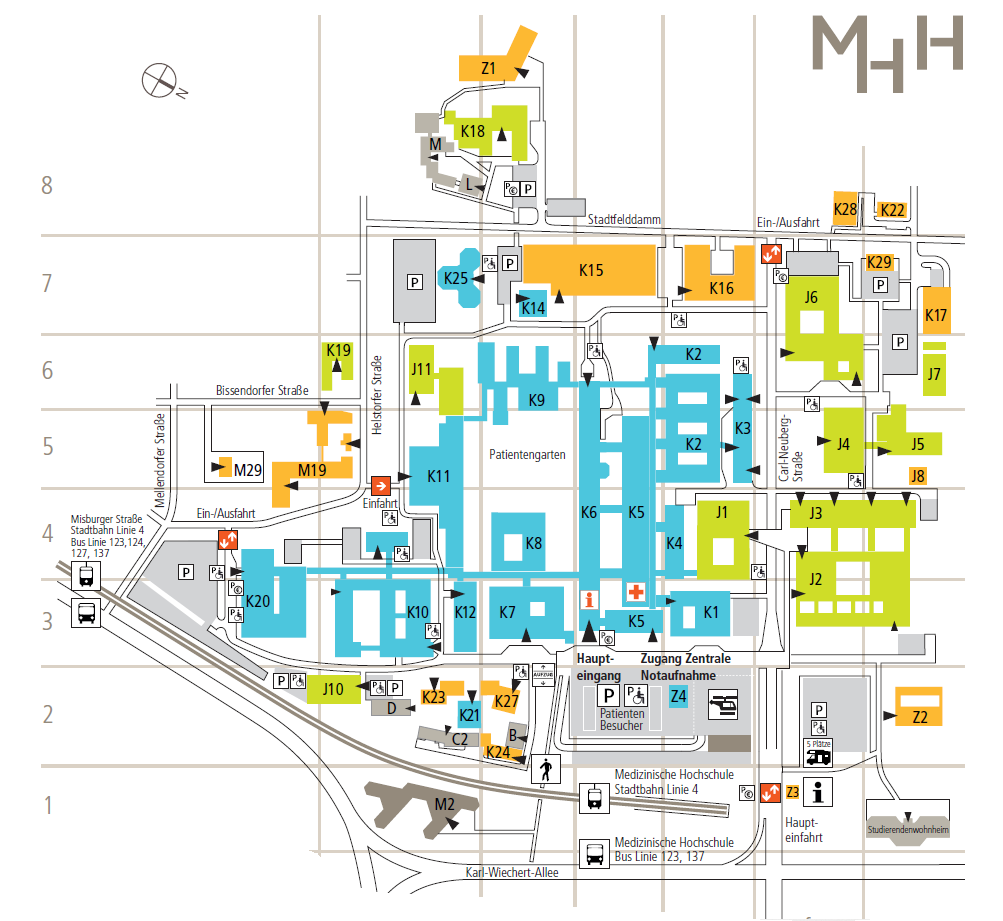
In OPAL, the Hannover Medical School cooperates with the AOK Lower Saxony, the Hameln-Pyrmont Health Region, the Schaumburg Health Region, the Lower Saxony General Practitioners' Association and the Lower Saxony State Support Center for Hospice Work and Palliative Care.
Funding
The project is funded by the Innovation Fund of the Joint Federal Committee for the area of health services research (funding reference 01VSF17028). The funding period ran from 01.07.2018 to 31.12.2021.
Publications
Afshar K, Müller-Mundt G, van Baal K, et al. Optimal care at the end of life (OPAL): Study protocol of a prospective interventional mixed-methods study with pretest-posttest-design in a primary health care setting considering the view of general practitioners, relatives of deceased patients and health care stakeholders. BMC Health Services Research. 2019; 19(1): 486. published 2019 Jul 15.(PubMed)
Afshar K*, van Baal K*, Wiese B, Schleef T, Stiel S, Müller-Mundt G, Schneider N. Structured implementation of the Supportive and Palliative Care Indicators Tool in general practice - A prospective interventional study with follow-up. BMC Palliative Care. 2022;21:214.(PubMed)
Schrader S, van Baal K, Schleef T, Schneider N, Afshar K, Müller-Mundt G. "...the classic problem is to say, you are palliative now" - end-of-life care at the interfaces to general practitioner care in rural regions - a qualitative multi-perspective study. Z Palliativmed 2020; 21(6): 309-315
van Baal K, Wiese B, Müller-Mundt G, Stiel S, Schneider N, Afshar K. Quality of end-of-life care in general practice - a pre-post comparison of a two-tiered intervention. BMC Prim Care. 2022; DOI: 10.1186/s12875-022-01689-9.(PubMed)
van Baal K, Schrader S, Schneider N, Wiese B, Stahmeyer JT, Eberhard S, Geyer S, Stiel S, Afshar K. Quality indicators for the evaluation of end-of-life care in Germany - a retrospective cross-sectional analysis of statutory health insurance data. BMC Palliative Care 2020; 19:187(PubMed)
van Baal K, Schrader S, Schneider N, Wiese B, Stiel S, Afshar K. Care of people at the end of life in a rural-small-town region of Lower Saxony: a retrospective cross-sectional analysis based on routine GP data. Z Evid Fortbild Qual Gesundhwes. 2022; DOI: 10.1016/j.zefq.2021.10.002(ScienceDirect)
van Baal K, Schrader S, Wiese B, Geyer S, Stiel S, Schneider N, Müller-Mundt G, Afshar K. GPs' perspective on End-of-Life Care - an evaluation based on the German version of the General Practice End of Life Care Index. GMS Ger Med Sci. 2020; 18:Doc10.(PubMed)
van Baal K, Stiel S, Hemmerling M, Stahmeyer JT, Wiese B, Schneider N, Afshar K. Outpatient palliative care in Lower Saxony - regional differences in the care of people at the end of life based on quality indicators. Central Institute for Statutory Health Insurance Physicians in Germany (Zi). Care atlas report no. 21/04. Berlin 2021; DOI: 10.20364/VA-21.04(versorgungsatlas.de)
Congress contributions (pdf)
OPAL - Contact
OPAL - Team:
Prof. Dr. Nils Schneider (Project Management)
PD Dr. Kambiz Afshar (deputy project manager)
Dr. Gabriele Müller-Mundt (Research Assistant)
Sophie Schrader (Research Assistant)
Dr. Katharina van Baal (Research Associate)
Tanja Schleef (Research Assistant)
Sonja Riedel-Schatte (Research Assistant)
Hannah Frerichs (study assistant)
Address:
Hannover Medical School
Institute ofGeneral Medicine and Palliative Medicine
Carl-Neuberg-Straße 1
30625 Hanover