ProPall
Proactive palliative care for elderly patients in the last phase of life
Background
The care of older people in the last phase of life is becoming increasingly important to society and will continue to grow in importance. Population forecasts assume that by 2050, around 88% of people dying in Germany will be over 75 years old [1].
Many of these people can benefit from good palliative care, with the aim of improving or maintaining the quality of life of those affected and their relatives [2, 3]. Older frail people with chronic illnesses in the last phase of life are therefore an important target group for the further development of palliative care [4].

Objectives
The overarching objective of the project is to improve palliative care in primary care by general practitioners in private practice in conjunction with the health services involved in providing care.
Sub-goals of ProPall are
- the analysis of the logics of action, decision-making processes and influencing factors underlying the initiation of general palliative care in GP practices,
- the development and testing of an intervention concept to promote proactive palliative care for elderly patients in the last phase of life for general practitioner care practice and
- the evaluation of the intervention concept with regard to practicability in everyday care and the improvement of the quality of care for elderly patients in the last phase of life from the perspective of their relatives, etc.
The project builds on the findings of the qualitative longitudinal study "End of life care for frail older patients in family practice (ELFOP)" (BMBF funding code: 01GY1120 [4, 5]).
Patient advisory board
In order to ensure that the patient and user perspective is adequately taken into account, the project will be supported by a patient advisory board. Interested volunteer citizens, members of the region's senior citizens' advisory council and members of regional patient and relatives' self-help groups are being approached to participate in the patient advisory council.
Methods
The ProPall research project is an intervention study with a pre-post design. Qualitative and quantitative methods of health services research are used in the individual project phases (mixed methods design).
The research project extends over a total period of 36 months and is divided into three main phases.
The main phases of ProPall are
(1) The preliminary as-is analysis of care practice is based on:
- Guideline-based interviews with GPs, their practice members and key personnel in health services central to the care of older people
- Analysis of anonymized routine data on the patient profile of the GP practices involved and selected indicators (hospitalization, place of death, etc.) of the care process in the last phase of life and
- Guideline-oriented interviews with relatives of deceased patients of the participating GP practices.
(2) The development/adaptation and testing of the intervention concept includes
- an introductory event for the participating GPs and members of their practice team
- multidisciplinary and cross-facility workshops to develop or adapt a tiered intervention concept
- Testing and adapting the intervention concept in the participating GP practices over a period of approx. 12 months
- Monitoring of the trial phase through three workshops with the participating GPs and members of their practice team as well as regular practice visits by members of the project team to reflect on the implementation experiences in the practice team.
(3) The intervention is evaluated on the basis of
- the summarizing analysis of the application experiences
- the comparative analysis of selected quality indicators of end-of-life care (see above) and
- interviews with relatives of deceased patients of the participating GP practices
Publications
-
Freihoff S, Tetzlaff F, Schneider N, Stiel S, Müller-Mundt G. "That is also our goal, that we treat these patients in calm waters" - Palliative care for older people with life-limiting illnesses in general practice: A qualitative study. Z Palliativmed. 2020; 21(05): 260-266
-
Tetzlaff F*, Freihoff S*, Schneider N, Müller-Mundt G. Recognizing and responding to palliative needs of older people in primary care. Results of testing a decision aid. Z Allg Med. 2021; 97(11): 451-456 (*shared first authorship)
Funding
The ProPall research project was funded as part of the BMBF's "Guidelines for the Promotion of Research in Palliative Care - Projects of Young Scientists" (BMBF funding code: 01GY1710).
ProPall - Team
Prof. Dr. Nils Schneider (Institute Director)
Dr. Gabriele Müller-Mundt (Project Management)
Fabian Tetzlaff (research assistant until 11/2020)
Daniela Wehrt (research assistant)
Silke Freihoff (research assistant until 08/2020)
ProPall - Project Office:
Phone: +49 511 532-8091
Fax: +49 511 532-161088
E-mail: propalliativ@mh-hannover.de
Address
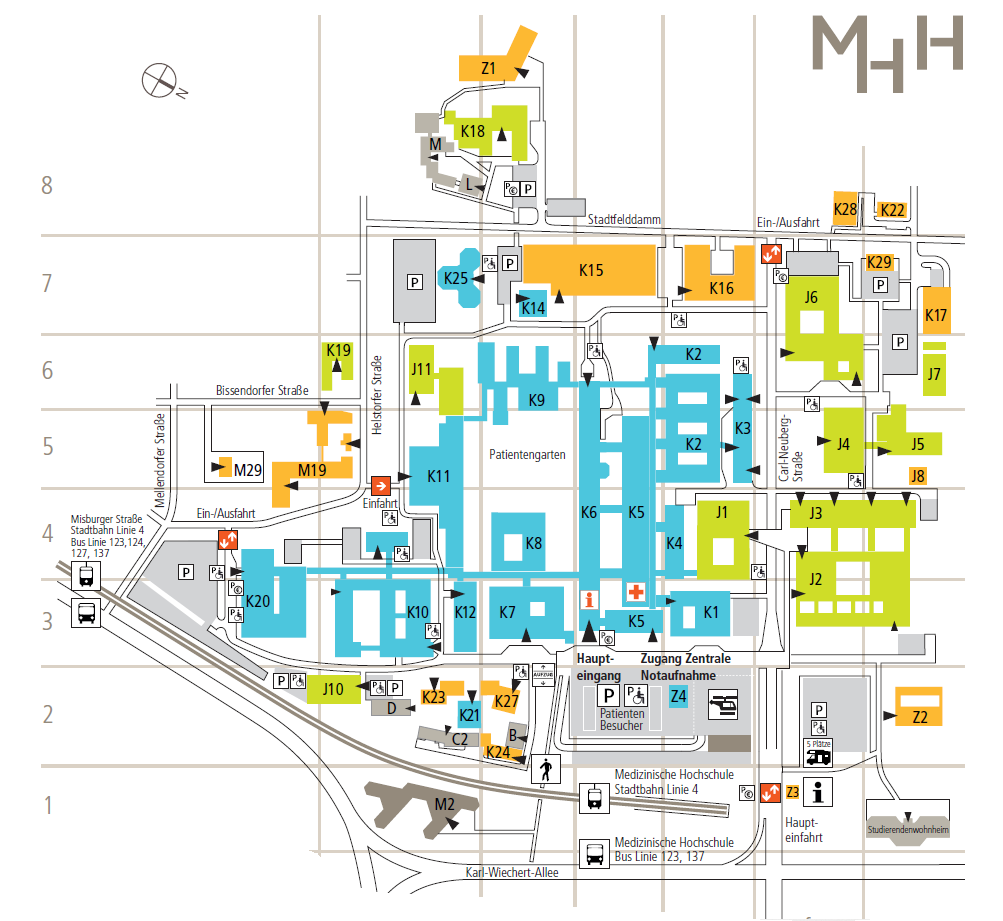
Hannover Medical School
Institute ofGeneral Medicine and Palliative Medicine
Carl-Neuberg-Strasse 1
30625 Hanover