Nutritional therapy
for hereditary fructose intolerance
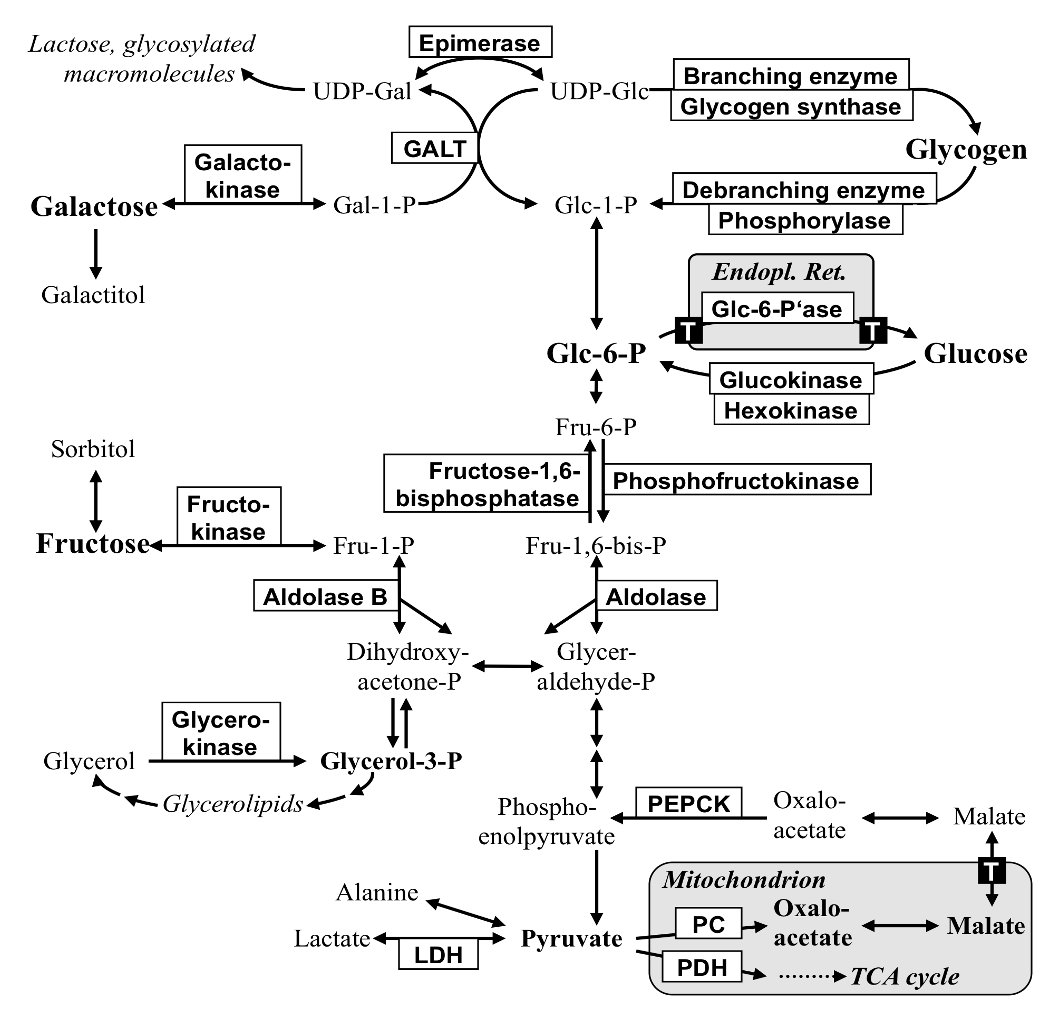
Hereditary fructose intolerance (HFI) is an autosomal recessive inherited metabolic disorder with a frequency of approx. 1:20,000. It is caused by a defect in the enzyme aldolase B, which converts fructose-1-phosphate to glycerol aldehyde and dihydroxyacetone phosphate in the liver. When fructose-containing foods or medications are ingested, fructose-1-phosphate accumulates and damages the liver, kidneys and intestines. Hypoglycaemia with symptoms such as nausea, vomiting, sweating, pallor, tremors, failure to thrive and gastrointestinal complaints become apparent, which in some severe cases have even led to death.
Getting the diagnosis right
HFI should not be confused with fructose malabsorption. In this case, there is a different enzyme defect in the mucous membrane of the small intestine. There are different enzyme defects and there are different dietary recommendations. An H2 breath test with fructose is not suitable for making a diagnosis, but puts the child's life at risk. HFI cannot be detected early in newborn screening, but in most cases patients become clinically conspicuous with the introduction of complementary foods. The diagnosis is then confirmed genetically. The diagnosis of HFI is made genetically by mutation analysis in the blood; alternatively, HFI can be diagnosed by detecting reduced aldolase activity in the small intestine or liver biopsy; these invasive diagnostic options are rarely used nowadays. If no fructose is ingested, patients have no symptoms. This condition persists in the first 5-6 months of life with exclusive feeding of breast milk or PRE infant formula. It is only when fructose in the form of fruit, vegetables, potatoes or household sugar is introduced with complementary foods or sugary teas/juices that the first symptoms become visible. Mothers are concerned because their children show signs of failure to thrive, gastrointestinal complaints, refusal to eat and an aversion to sweets. Not only fruit, fruit juices and vegetables, but also sweets are rejected by the children. In most cases, the pediatrician is then consulted for clarification and HFI is suspected. The dietary history is crucial for such descriptions of food choices and leads to diagnostic clarification using molecular genetics.
Correct treatment
The therapy is purely dietary. There are foods (LM) that do not contain fructose and can be eaten without restriction. Foods that contain little fructose are still well tolerated in small quantities, but foods with a lot of fructose must be avoided.
Fig. Food selection for hereditary fructose intolerance
Patients with HFI can achieve a good nutrient supply by avoiding foods high in fructose and taking a vitamin supplement. Supplementation of minerals is not necessary. The pharmacist can recommend a suitable vitamin supplement, as it must be free from fruit extracts, sugar, fructose, sorbitol and isomalt. Depending on your health insurance and with a physician's certificate, you can try to find out whether the costs will be covered by your health insurance. Although the choice of food limits plant and fiber-rich foods and increases the proportion of animal foods, the fat intake and the proportion of saturated fatty acids can be limited by giving preference to low-fat animal products.
In nutritional advice, parents are not advised to calculate fructose intake. Nevertheless, a list with 1 g of fructose in vegetables, bread, potatoes and cereals is helpful in recognizing large and small fructose suppliers and combining them accordingly. Such lists are available to members of the Pediatric Dietetics Working Group (APD).