MHH receives three million euros for research on artificial blood cells to counter shortages of blood reserves
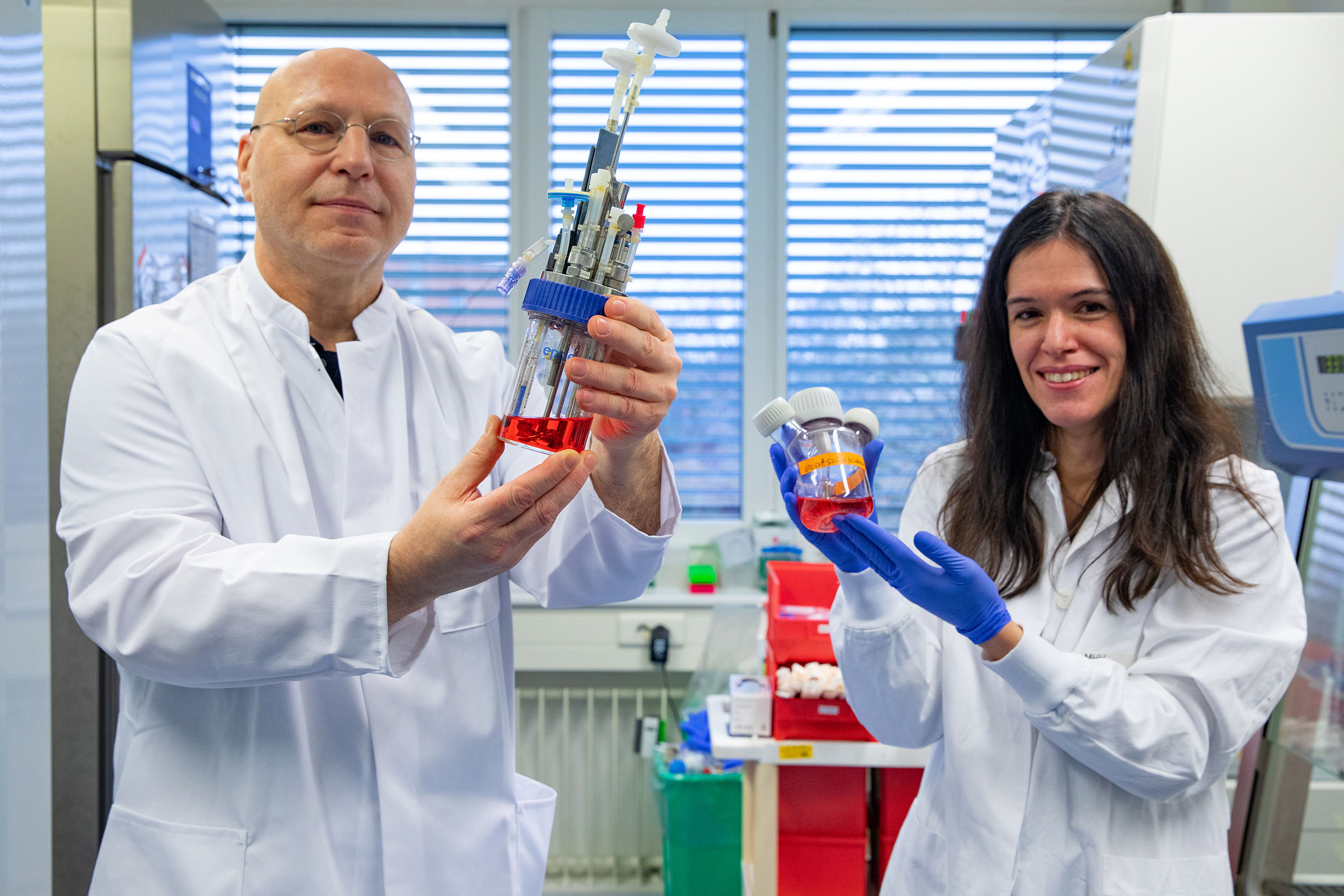
Professor Dr. Constanza Figueiredo and Professor Dr. Rainer Blasczyk with bioreactors for blood cell production in a laboratory of the Institute of Transfusion Medicine and Transplant Engineering; Copyright: Karin Kaiser / MHH
25.02.2022
Blood transfusions are among the most common procedures in hospitals. According to the German Red Cross, around 15,000 blood donations are needed every day in Germany alone. But only about four percent of potential blood donors actually donate blood - and the trend is downward. At the same time, the need for blood products is increasing because the number of available donors continues to decline due to the ageing population, while at the same time the age group over 60 has the highest consumption of blood products.
A research team led by Professor Dr Rainer Blasczyk, head of the Institute for Transfusion Medicine and Transplant Engineering at the Medical School (MHH), wants to solve this problem. The aim is to use molecular biological methods to produce specially adapted blood cells from stem cells and thus eliminate supply bottlenecks. The "Hemoforce" project is being funded by the Federal Ministry of Defence with more than three million euros for an initial period of four years.
Better tolerance without antigens
"In many regions of the world, blood reserves are already in short supply," says Professor Blasczyk. In addition, he says, it is not always easy to transport fresh blood to where it is currently needed. But even if it is available, donated blood does have disadvantages. For example, it is not only the different blood groups that have to be taken into account in a transfusion. Tissue characteristics, the so-called human leukocyte antigens (HLA), also play a role. These molecules on the surface of body cells are comparable to the blood group antigens on red blood cells and differ individually from person to person. In a stem cell transplant, the HLA characteristics must be as similar as possible so that the recipient's immune system does not reject the donor cells. Even after a transfusion, platelets that do not have matching HLA proteins can be recognised and destroyed by components of the recipient's immune system. Another problem with conventional blood products is possible pathogens, as blood cannot be tested for all pathogens and, moreover, all test methods have a detection limit.
Unlimited production in the bioreactor
"The disadvantages of conventional blood donations make it urgent to redesign the model and structures of the blood supply," emphasises the transfusion physician. For about 30 years, scientists worldwide have already been working on "blood pharming", i.e. the artificial production of blood products. However, mass production for clinical use is not yet in sight.
The MHH project is initially concentrating on so-called megakaryocytes. These blood-forming cells are mainly found in the bone marrow and develop into platelets, which are important for blood clotting. The research team produces them in cell culture from induced pluripotent stem cells (IPSC). These are genetically reprogrammed body cells that have similar properties to embryonic stem cells, i.e. they can develop into all types of tissue. This method paves the way for unlimited production of artificial blood cells in the bioreactor.
Megakaryocyte cells produce platelets in a mouse model
"We obtain the iPSCs from reprogrammed cells of a human with blood group zero, which is an ideal donor group that does not carry AB0 antigens and is therefore equally suitable for all recipients," explains Professor Dr. Constanca Figueiredo, senior scientist at the Institute and deputy project leader. In addition, the scientist genetically modified the iPSC and also switched off the HLA characteristics of the cells. The result is a kind of blueprint for "neutral" megakaryocyte cells that are no longer recognised as foreign by the recipient's immune system and can thus produce platelets undisturbed without the body forming antibodies against them.
The research team has already proven that the approach works in the mouse model. "Just one hour after the transfusion, the megakaryocyte cells started to produce platelets very sustainably," says Professor Figueiredo. The scientist is convinced that this should be equally successful in humans. "A living body is always the best bioreactor." There is no danger of the donor cells degenerating and forming tumours. "The megakaryocyte cells are irradiated before transfusion and can therefore no longer divide, but only produce platelets," explains Professor Blasczyk. The platelets themselves do not have a cell nucleus anyway, so they cannot reproduce independently by nature.
Solving storage problems
Another aspect is the storage of the blood cells. Up to now, blood reserves and cell products have been deep-frozen in liquid nitrogen to make them last longer. In order for the cells to survive this, glycerine, among other things, is added to the blood reserves, which has to be removed again before the transfusion. Together with Professor Dr. Willem Wolkers from the Lower Saxony Centre for Biomedical Engineering, Implant Research and Development (NIFE), new cryotechniques are to be developed.
"We want to find cryoprotectants without toxic side effects that make time-consuming cleaning unnecessary and also allow storage at higher temperatures," says Professor Blasczyk. In the second funding phase, the research team wants to move into mass production of the artificial blood cells and conduct the first clinical trials on humans.
SERVICE:
For further information, please contact Professor Dr. Rainer Blasczyk, blasczyk.rainer@mh-hannover.de, phone (0511) 532-6700.