MHH researchers have found biomarkers that predict which patients will benefit from treatment with checkpoint inhibitors.
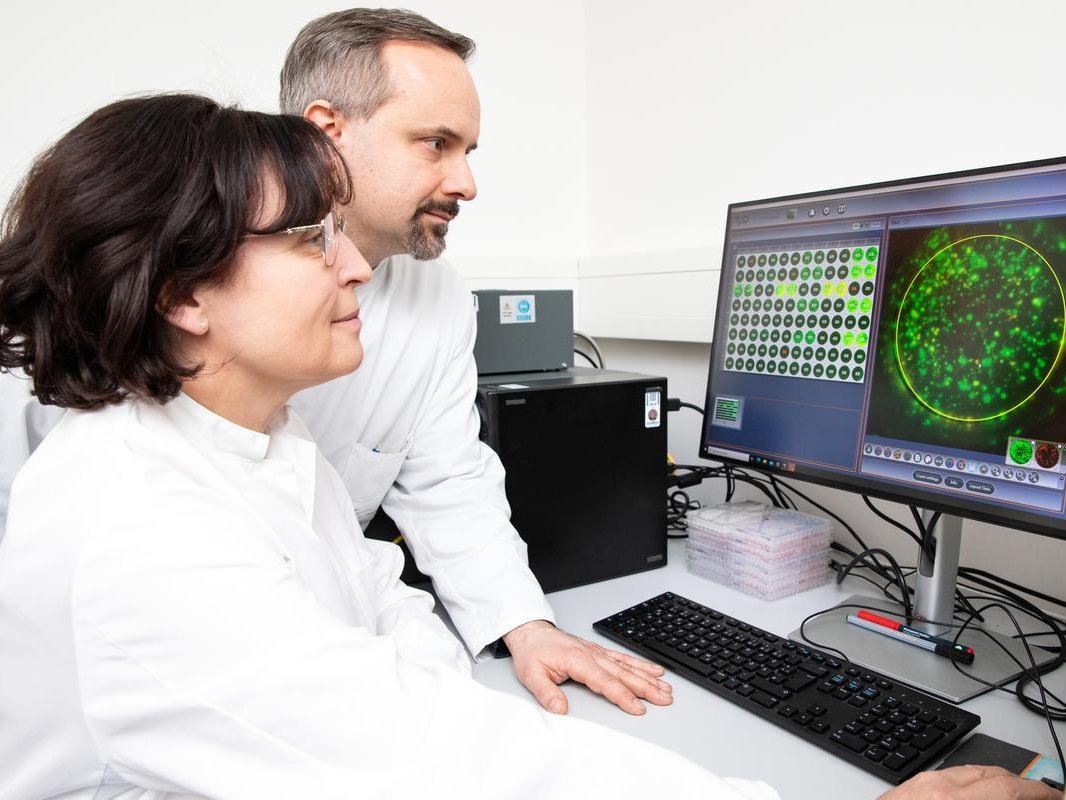
Prof. Dr. Britta Eiz-Vesper and Prof. Dr. Thomas Skripuletz analyze the results of a test that makes virus-specific T cells visible in the blood of a PML patient. Copyright: Karin Kaiser/MHH
Progressive multifocal leukoencephalopathy (PML) is a rare but serious brain infection. It gradually destroys the brain tissue and often leads to death within a few weeks. It is caused by the human polyomavirus 2 - also known as John Cunningham (JC) virus. At its core, PML affects people with weakened immune cells, especially T lymphocytes. One treatment option is the use of so-called immune checkpoint inhibitors (ICI). This therapy, known from cancer medicine, switches the immune system back on, so to speak. However, the treatment is not always successful and can also have serious side effects. It is not yet possible to predict which patients will benefit from ICI therapy and which will not. An interdisciplinary team at Hannover Medical School (MHH) led by Prof. Dr. Thomas Skripuletz, senior physician at the Clinical Department of Neurology with Clinical Neurophysiology, has now found biomarkers that can predict a response to immunotherapy. The results of the study have been published in the journal "JAMA Neurology".
Higher response rates, longer survival
In their study, the researchers evaluated 111 PML patients from 39 Clinical Departments worldwide who were treated with ICI between 2021 and 2024. Before starting treatment, they were able to check the blood of some of the patients to see whether functional, virus-specific T cells against the JC virus were present or not. They then examined both groups and compared, among other things, how the patients responded to the ICI therapy, how much virus could be detected in the cerebrospinal fluid, what side effects the treatment had and how long the survival time was. "We were able to observe that PML patients with virus-specific T cells that were detectable before the start of treatment had significantly higher response rates, better functional progression, lower viral loads during the course and a better probability of survival during and after ICI treatment," emphasizes Professor Skripuletz. "At the same time, they experienced fewer immune-mediated side effects."
Precisely matched T cells thanks to the alloCELL donor register
This result is of great importance, as ICI therapy is the only treatment option for PML in most Clinical Departments worldwide. However, there is another treatment option at the MHH. In 2021, Professor Skripuletz and his team found a groundbreaking way to stop the spread of the virus with the help of donated, precisely matched immune cells. These directly isolated, so-called allogeneic DIAVIS T cells come from the blood of healthy people who were often infected with the virus without developing symptoms of the disease. They have T cells that recognize JC virus-infected cells as foreign and trigger an immune response. "However, before we administer virus-specific T lymphocytes from donors by infusion, we always analyze whether the patient's own T cells directed against the virus are still detectable in the blood," says Professor Skripuletz. However, most patients are not eligible for checkpoint inhibitors because they lack these cells - in this case, they benefit from treatment with donor T cells.
The alloCELL laboratory at the MHH in Hanover analyzes the presence of virus-specific T cells. "Thanks to our unique alloCELL T-cell donor register at the MHH, we always find a suitable T-cell donation if no immune cells of our own are available," emphasizes Prof. Dr. Britta Eiz-Vesper, immunologist at the MHH Institute of Transfusion Medicine and Transplant Engineering and co-author of the study. The alloCELL register not only collects the tissue characteristics of the blood cells, but also the number of specific T cells against different viruses. Because the Institute is also one of Germany's leading manufacturers of virus-specific T cells, suitable donors can be found quickly and the T cell products can be made available for treatment within a few days of the request. "We send the T cells to all possible centers in Germany and abroad," says the immunologist.
Blood test recommended before ICI therapy
Nevertheless, ICI therapy plays an important role worldwide. "For the first time in a larger cohort, our data provide evidence that a blood test for virus-specific T cells could be suitable as a biomarker," says Professor Skripuletz. This test can identify PML patients in whom checkpoint inhibitors are particularly likely to be effective and better tolerated. "The study underlines the central role of pre-existing antiviral immunity and confirms that T cells directed against the JC virus can guide clinical decisions in this rare but highly relevant neuroinfectious disease." The aim is to make this examination the standard before starting therapy.
SERVICE:
The original paper "Virus-Specific T Cells and Response to Checkpoint Inhibitors in Progressive Multifocal Leukoencephalopathy" can be found here.
Text: Kirsten Pötzke