Bladder dysfunction
The diagnostics should verify the presence of a bladder dysfunction and determine its severity, type and cause. The following examinations are used:
- General, micturition and incontinence history: a loss of urine when coughing, sneezing, laughing or during physical activity is most likely to indicate stress incontinence. Loss of urine with the urge to urinate, often in a resting position or with running water, is more likely to indicate urge incontinence.
- Medication history: Medications that affect the autonomic nervous system can influence bladder function.
- Micturition diaries are used to objectively record micturition frequency and urinary incontinence and are also used to monitor treatment.
- In addition to the general physical examination, the lower abdomen and genitals should also be examined. Any abnormalities in the neurological examination should prompt further neurological diagnostics.
- A urinary tract infection should be ruled out before any extensive diagnostics.
- An ultrasound examination of the urinary bladder reveals bladder stones, foreign bodies or bladder tumors. A sonographic examination of the upper urinary tract is used to rule out urinary retention, which is mainly observed in cases of overflow incontinence or neurogenic bladder dysfunction, as well as urolithiasis, which can cause a urinary tract infection.
- In women, in addition to abdominal sonography, perineal, introitus, vaginal or rectal sonography is also used to visualize the position of the bladder neck and the shape and position of the urethra in relation to the bladder neck.
- Clinical incontinence tests are used to answer specific questions. The pad test objectively quantifies the amount of urine loss. The cough test is used to diagnose the type of incontinence. With stress incontinence, urine loss occurs when coughing, with urge incontinence regardless of coughing.
- Urinary stream measurement (uroflowmetry) and residual urine measurement should be carried out initially in all patients to rule out a bladder emptying disorder.
- The urodynamic examination (bladder pressure measurement) alone makes it possible to reliably diagnose the type of incontinence.
The subcutaneous implantation of a small pacemaker system is a long-term therapeutic option for the treatment of various pelvic floor dysfunctions. Gentle electrical impulses to the sacral nerves modulate the transmission of information between the brain and pelvic floor organs in such a way that the natural function of the bladder (and also the rectum) can be restored.
The treatment consists of two parts:
- The test phase: in this phase, only the electrodes are implanted to check the clinical response and the patient's handling of the system
- The definitive implantation: after a successful test phase, the pulse generator is positioned in a subcutaneous pocket on the buttocks.
The patient receives a remote control, which enables customized programming.
Suitable for:
- Overactive bladder (OAB) with or without urge incontinence
- Detrusor underactivity or dysfunctional micturition
- Chronic pelvic pain (pelvic pain syndrome)
- COMBINED FUNCTIONAL DISORDERS (e.g. urge incontinence, faecal incontinence, urinary retention, chronic constipation, etc.)

Urinary incontinence in men
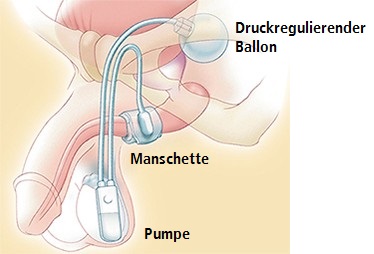
The implantation of an artificial sphincter (artificial sphincter, AMS 800®) is the surgical method of choice for men. This prosthesis, which is made of silicone and then filled with fluid, consists of three components:
- inflatable closure sleeve,
- pressure-regulating balloon and
- control element with pump.
The sealing sleeve is placed around the bulbar urethra. Pressure on the pump transports the fluid from the cuff into the balloon. The return flow of fluid is delayed for three to five minutes by a valve in the control element. The cuff remains open during this time while the patient empties the bladder. The AMS 800® is an effective method for treating stress incontinence, which leads to continence success in 82 to 100 percent of patients.
Advantages:
- For every degree of incontinence
- Even if the sphincter muscle is injured or no longer active
- Even after radiotherapy of the pelvic region
- Complete urethral closure
Contraindications:
- Difficult or impossible handling (e.g. Parkinson's disease or disabilities)
- Further transurethral procedures planned (e.g. aftercare of superficial bladder tumors)
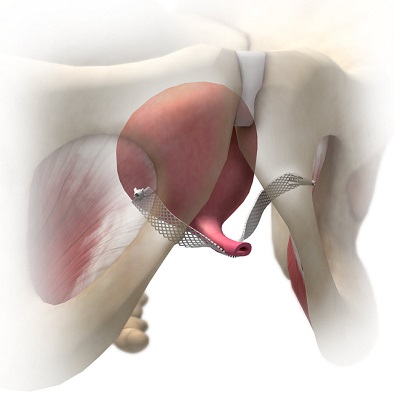
Similar to the placement of the suburethral slings, the ATOMS system also involves the transobturator insertion of the retaining strap, which is also attached around the lower pubic ramus on both sides. The filled silicone cushion increases the discharge resistance by compressing the bulbospongiosus muscle - and thus indirectly the urethra. Individual adjustment is possible at any time and without surgery by refilling the cushion through the port.
Advantages:
- Suitable for mild to moderate urinary incontinence
- Also after radiotherapy of the pelvic region
- No manual operation
- Further transurethral interventions possible
Contraindications:
- Total urinary incontinence
- Injured or no longer functioning sphincter muscle
Results:
- Success rate of 77.7 - 93.8 % with dryness up to 64 %
- Up to 20 % explantation rate, mostly due to titanium intolerance
Urinary incontinence in women
In total, there are more than 200 surgical procedures available for the treatment of female stress incontinence. All of them are aimed at improving pressure transmission and/or increasing urethral closure pressure. For a long time, suspension plasty was the standard operation for female stress incontinence in Germany, as long-term results with high continence rates are available. The principle of suspension is based on shifting the urethra and bladder neck upwards and forwards in order to improve pressure transmission under stress.
Tension-free tapes (so-called TVT or TOT) are nowadays preferred in Germany due to the quick, simple and uncomplicated surgical technique. The mechanism of action of the implanted tension-free tapes is based on the creation of a hard resistance in the middle of the urethra, which leads to kinking of the posterior urethra under stress. Randomized studies comparing the effectiveness of Burch and TVT operations or TVT and TOT operations have shown that the continence rates of the individual surgical methods do not differ significantly.
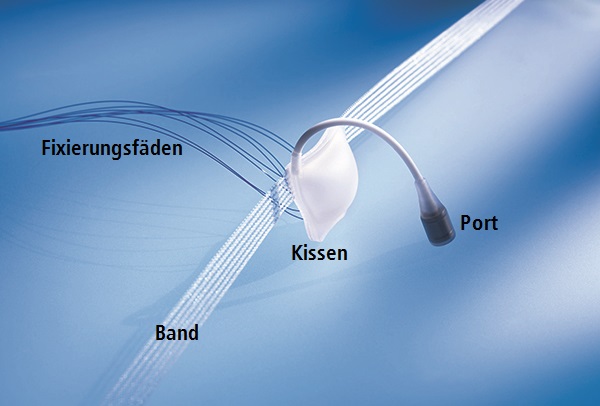
The tension-free tapes:
- Tensionfree Vaginal Tapes (TVT® ): in this surgical method, a polypropylene tape is placed tension-free on the front of the mid urethra. A trocar is used to pierce the pelvic floor, first on the left and then on the right, and the tape is pulled up through the lower abdomen to the side of the bladder.
- Alternatively, the tape can also be passed through the obturator fossa to the anterior vaginal wall, thus avoiding bladder, bowel and vascular injuries (so-called TOT® or TVT-O® technique).
- Since 2007, a new band system has been available which is implanted transvaginally via a single incision (SIMS, Single-Incision Mini-Sling). This system can be implanted with virtually no bleeding and within a very short time (approx. 5 to 10 minutes). Short-term results of up to twelve months are comparable to those of TVT® and TOT®.