SPICT
Identification of patients with palliative care needs in hospitals and practices
Background
Patients with chronically progressive diseases can develop problems and symptoms during the course of their illness that make palliative care appropriate. However, in the day-to-day care of hospitals and physicians' practices, it is often difficult to adequately recognize the time for palliative care.
International studies and our own preliminary work underline the need for a structured assessment. No empirically tested instrument is yet available for this in Germany. In contrast, the Supportive and Palliative Care Indicators Tool (SPICT ), developed and tested empirically by the Primary Palliative Care Research Group at the University of Edinburgh under the leadership of Dr. Kristy Boyd and Prof. Scott Murray, is used internationally. In 2015/16, an Austrian-German working group produced the first German-language translation of the tool (SPICT-DE™). However, this has not yet been systematically tested and evaluated in practice.
Study question and objectives
The aims of our ongoing pilot studies are to adapt the language and test a German-language version of SPICT to test its practicability, acceptance and relevance in inpatient and outpatient care settings. Qualitative and quantitative healthcare research methods are used (mixed methods design).
However, scientific studies have shown that the integration of palliative care into the daily routine of general practitioners is a challenge. There is therefore a need for more in-depth research into how the implementation of palliative care by GPs can be facilitated.
Methodological approach and initial results
The systematic empirical review and adaptation of SPICT-DE™ is carried out in cooperation and close exchange with the originators of the instrument. The procedure is based on the TRAPD model tried and tested in transcultural research: Translation - Review - Adjudication - Pretest - Documentation (see also "Guidelines for Best Practice in Cross-Cultural Surveys, available at: http://www.ccsg.isr.umich.edu/images/PDFs/CCSG_Full_Guidelines_2016_Version.pdf.
Qualitative and quantitative methods of health services research are used accordingly (mixed methods design).
Initial results in the inpatient setting indicate that the use of SPICT sensitizes clinicians to palliative care situations in patients on normal internal medicine wards (Afshar et al. 2015). Further trials are underway in the outpatient GP setting.
Publications and further information
- Afshar K, Wiese B, Schneider N, Müller-Mundt G. Systematic identification of critically ill and dying patients in primary care using the German version of the Supportive and Palliative Care Indicators Tool (SPICT-DE). GMS Ger Med Sci. 2020; 18: Doc02
- Afshar K, Feichtner A, Boyd K et al. Systematic development and adjustment of the German version of the Supportive and Palliative Care Indicators Tool (SPICT-DE). BMC Palliative Care. 2018; 17: 27 (PubMed)
- Afshar K, Müller-Mundt G, Schneider N. How can patients with chronic progressive non-oncological diseases be identified for whom palliative care is appropriate? A pilot study to test the Supportive and Palliative Care Indicators Tool (SPICT) in hospital. Z Palliativmed. 2016; 17: 133-138
-
SPICT homepage: www.spict.org.uk
Funding
University-internal performance funding (HiLF) of Hannover Medical School, own funds
SPICT - Project team and contact
PD Dr. med. Kambiz Afshar (Project Manager)
Phone: +49 511 532-5855
E-mail: afshar.kambiz@mh-hannover.de
Dr. PH Gabriele Müller-Mundt
Prof. Dr. med. Nils Schneider
Address
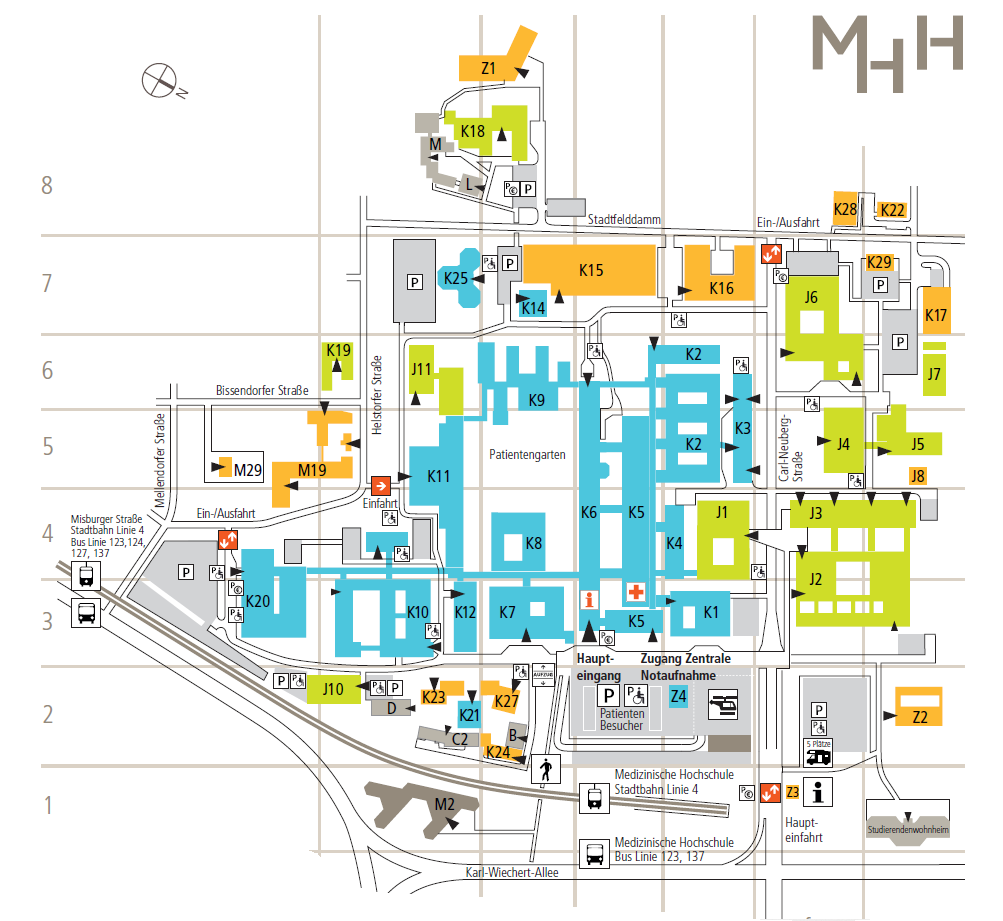
Hannover Medical School
Institute ofGeneral Medicine and Palliative Medicine
Carl-Neuberg-Strasse 1
30625 Hanover