Severe courses of various diseases can lead to organ failure. Individual or multiple organ systems can be affected. In this situation, organ replacement procedures are the only way out and replace the organ function.
Whether due to a serious infection, a congenital metabolic disease, an accident or a congenital heart defect, for example, it is sometimes not possible to maintain organ function - in which case organ failure occurs. If only one organ is affected, this is known as kidney failure or lung failure, for example; if several organs are affected, this is known as multiple organ failure. How long an organ failure lasts is influenced by various things, including the cause. And this often determines whether the organ can recover or not.
Organ replacement procedures bridge critical phases - until recovery or transplantation.
Intensive Care Unit 67 offers all established organ replacement procedures. A special therapy concept for cardiopulmonary support is awake ECMO, a procedure that allows the patient to be awake and communicative - even if the circulation or lungs require invasive support. In the following sections you will find a brief overview of the relevant procedures:
More information on ECMO procedures (heart) lung support More information on dialysis (kidney support) and MARS (liver support)
(Heart) lung support - ECMO
Veno-arterial extracorporeal membrane oxygenation (VA-ECMO)
Venoarterial circulatory replacement in children using ECMO/ ECLS (= Extracorporeal Membrane Oxygenation/ = Extracorporeal Life Support) is the treatment of choice for cardiopulmonary failure that cannot be managed conservatively. In addition to the classic ECMO indications such as cardiogenic shock (e.g. fulminant myocarditis, decompensated heart failure), it can also be used for non-cardiac shock (e.g. sepsis, meconium aspiration, neonatal diaphragmatic hernia, persistent pulmonary hypertension of the newborn).
Veno-venous extracorporeal membrane oxygenation (VV-ECMO)
In cases of respiratory failure that cannot be managed conservatively, e.g. in the context of severe viral infections (influenza pneumonia), veno-venous ECMO in the sense of extracorporeal lung replacement is an established treatment option. The use of ECMO can reduce high ventilation parameters and promote lung recovery.
Long-term support - using awake ECMO
With the routine use of centrifugal pumps and completely heparin-coated tip-to-tip systems, a comparatively safe application over days and weeks is possible. A significant advance in patient care is the successful establishment of the "awake ECMO concept" in pediatric patients as well. In addition to constant neurological assessment of the patient, the aim is to avoid complications associated with intensive care (protracted weaning, ventilator-associated pneumonia, critical illness polyneuropathies). In some patients, awake ECMO allows extensive mobilization on the extracorporeal system and the implementation of physiotherapeutic measures.
ECMO perioperatively during lung transplantation for pulmonary hypertension
If there is a risk of right heart failure in the terminal stage of pulmonary hypertension, VA-ECMO can be applied percutaneously without risky anesthesia (including antegrade leg perfusion). After transplantation, ECMO primarily supports the left ventricle in adapting to the postoperative increased volume load. This concept has significantly improved the survival rate.
A working group in intensive care unit 67 is scientifically investigating improvements to ECMO procedures and incorporating the findings into current therapies.
More information on the ECMO working group
Dialysis procedures - kidney and liver support
Renal replacement - dialysis procedures
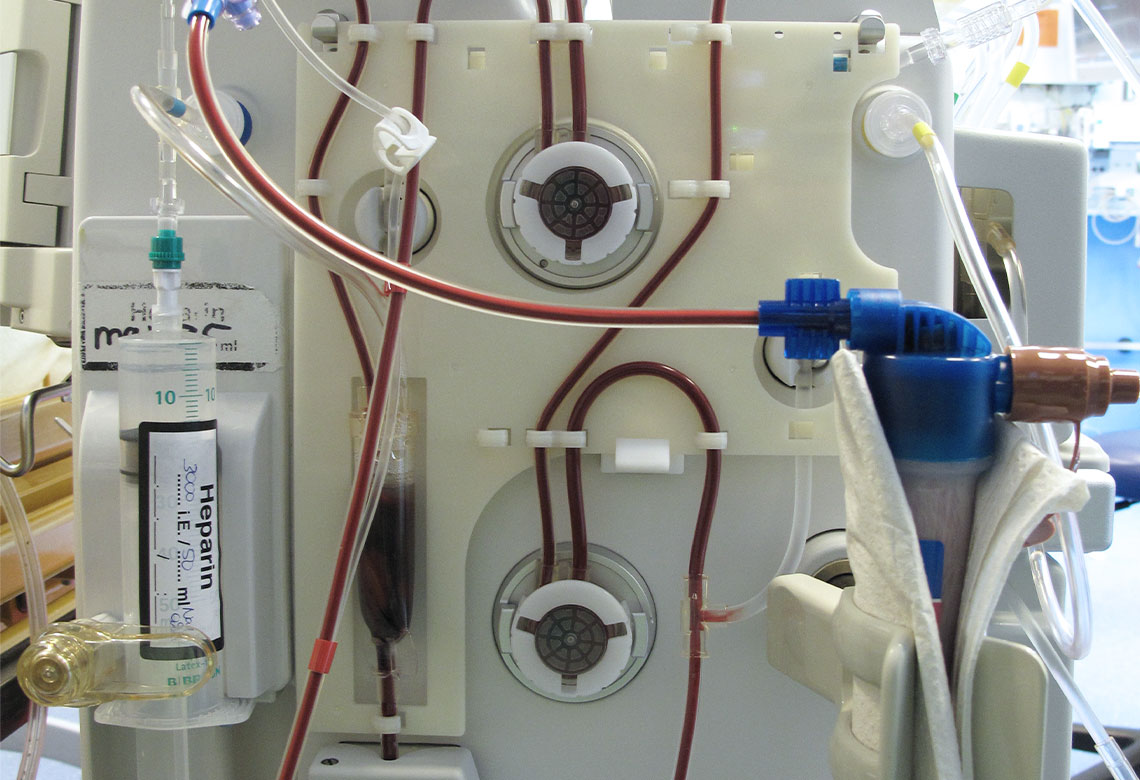
In addition to extracorporeal cardiovascular replacement, there is also the option of renal replacement therapy - dialysis - in close cooperation with our pediatric nephrologists from the KfH (Kuratorium für Hämodialyse).
All standard dialysis procedures can be offered on intensive care unit 67:
- Hemodialysis
- haemodiafiltration
- haemofiltration
- Peritoneal dialysis
Dialysis is an integral part of intensive medical care for our sick patients, particularly in cases of severe disease progression with temporary loss of kidney function. The various dialysis procedures are also used to eliminate toxins in cases of intoxication (poisoning) or for specific immunotherapy.
Liver support - MARS or SAPD
In the event of acute liver failure, liver dialysis using so-called MARS therapy (Molecular Adsorbents Recirculation System) or Single Pass Albumin Dialysis (SAPD) is possible in cooperation with the Department of Pediatric Nephrology and Gastroenterology. Similar to renal replacement therapy, these very specialized therapies are intended to provide at least some replacement for parts of liver function. In selected cases, these therapies can be used in an attempt to bridge the time until a liver transplant is necessary.