More news on the homepage
Additive therapeutic plasma exchange in septic shock
Sepsis is the most severe form of any infection. Septic shock (sepsis with severe circulatory failure) is the main cause of death of patients in (non-cardiac) intensive care units. Septic shock and the associated multi-organ failure are triggered by an excessive reaction of the human organism to the initial infection. Cleansing the blood to treat this pathological reaction directly is therefore a tempting therapeutic concept.
Last year, the "Translational Intensive Care Medicine" working group reported the results of a randomized, controlled pilot study in which an additive Therapeutic Plasma Exchange (TPE) was investigated in patients with severe refractory septic shock. In this study, 40 patients with early (< 24 hours) and severe (noradrenaline dose > 0.4 μg/kg/min) septic shock were randomized to standard therapy or a single TPE with plasma as a substitution solution. A rapid hemodynamic improvement was observed in the TPE compared to the control group. These results were published in the renowned journal Intensive Care Medicine.
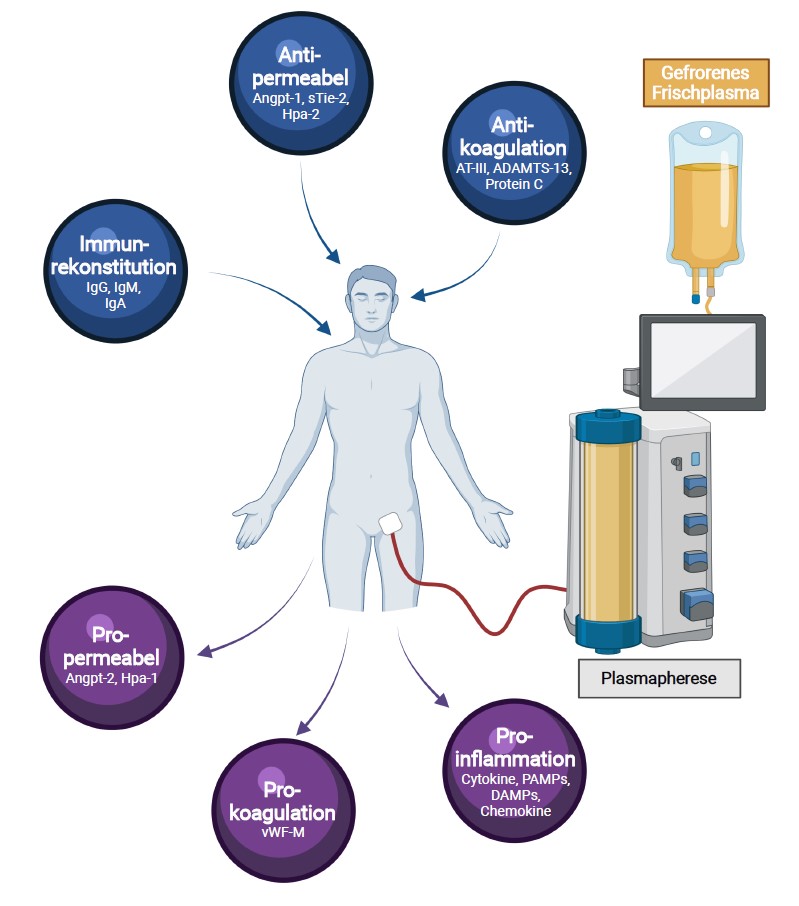
Potential molecular explanations as to why TPE leads to rapid circulatory stabilization in early and severe septic shock, and indications as to exactly in which patients this is to be expected, have now been revealed by a further study by the same research team, which was recently published in the journal Critical Care. TPE combines two therapeutic measures in a single procedure: on the one hand, it effectively removes harmful mediators such as pro-inflammatory cytokines, endothelial destabilizing factors (e.g. angiopoietin-2, sTie2, heparanase-1) and molecules involved in intravascular coagulation (e.g. von Willebrand factor). At the same time, the exchange of septic plasma with plasma from healthy donors leads to a replenishment of protective factors involved in anti-inflammatory processes (e.g. immunoglobulins), endothelial stabilization (e.g. angiopoietin-1, heparanase-2) and endogenous coagulation inhibition (e.g. antithrombin-III, protein C, ADAMTS-13), which are already depleted in the early phase of sepsis. It is therefore possible that TPE leads to an improvement in blood flow in the small vessels (so-called microcirculation) in a variety of ways. Interestingly, patients with the highest lactate blood concentrations (signs of the most severe microcirculatory disorder) in particular benefited from the initiation of additive treatment with TPE.
However, the benefit of additive TPE in septic shock in terms of patient survival remains unclear. A larger randomized study, which will investigate the additive use of TPE in septic shock, is already being planned jointly by a team from the Medical School (MHH, PD Dr. K. Stahl), the University Hospital Bonn (UKB, PD Dr. C. Bode) and the University Hospital Zurich (USZ, Prof. Dr. S. David) (EXCHANGE study with the participation of 22 centers in Germany and Switzerland).
For further information, please contact PD Dr. Klaus Stahl, stahl.klaus@mh-hannover.de, phone 0511-532-3305
To the original article:
1. clinical and biochemical endpoints and predictors of response to plasma exchange in septic shock: results from a randomized controlled trial. Stahl K, Wand P, Seeliger B, Wendel-Garcia PD, Schmidt JJ, Schmidt BMW, Sauer A, Lehmann F, Budde U, Busch M, Wiesner O, Welte T, Haller H, Wedemeyer H, Putensen C, Hoeper MM, Bode C, David S. Crit Care. 2022 May 12;26(1):134. doi: 10.1186/s13054-022-04003-2. PMID: 35551628 Free PMC article. Clinical Trial.
2 Adjuvant therapeutic plasma exchange in septic shock: David S, Bode C, Putensen C, Welte T, Stahl K; EXCHANGE study group. Intensive Care Med. 2021 Mar;47(3):352-354. doi: 10.1007/s00134-020-06339-1. Epub 2021 Jan 20. PMID: 33471132 Free PMC article. No abstract available.
