Description
Aortic isthmus stenosis (ISTA) is a common heart defect (6-10% of all heart defects). It is a malformation of the aorta close to the heart. In most cases it occurs in isolation, but may be accompanied by other abnormalities of the heart. 20-30% of cases of ISTA are associated with a ventricular septal defect, a malformation of the aortic valve, a narrow arch of the aorta or other complex cardiac abnormalities.
Occasionally, other genetic defects such as chromosomal abnormalities occur (monosomy X - Turner syndrome).
Anatomy
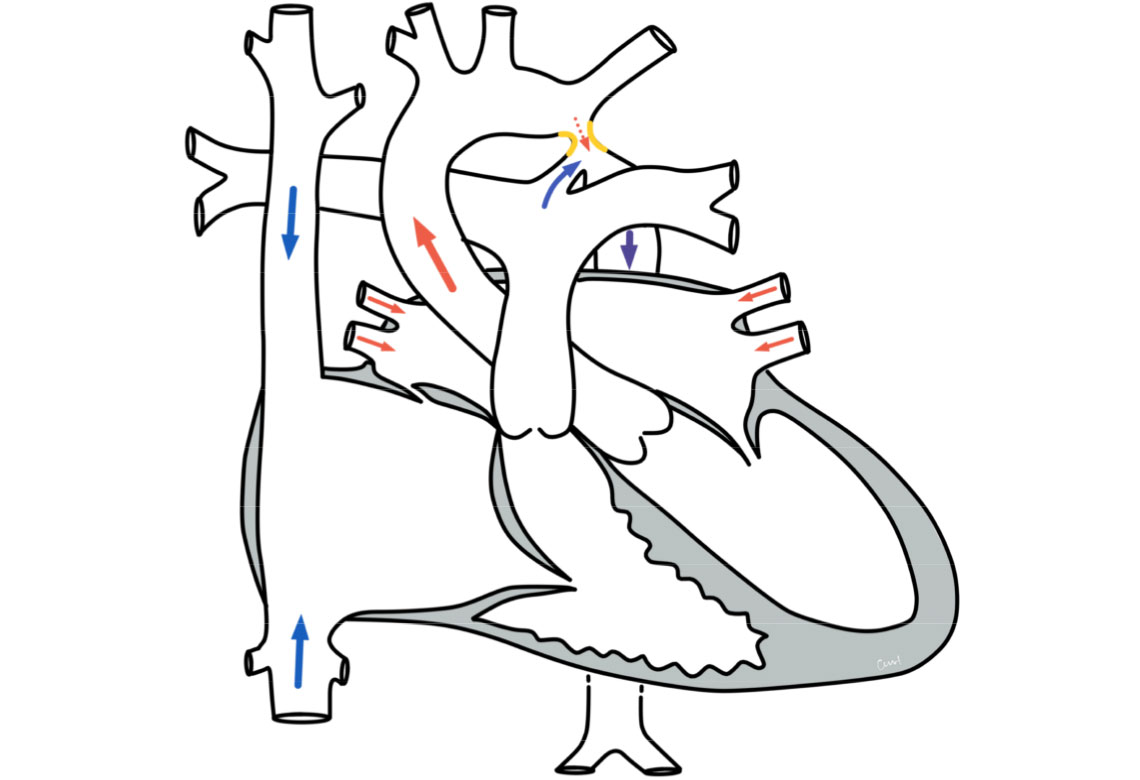
ISTA is characterized by a narrowing (stenosis) at the end of the arch of the aorta. This narrow area is located in the descending part of the aorta, shortly after the exit of the head and neck vessels. This area is called the isthmus and is usually located at the junction of the so-called ductus botalli. The ductus botalli is a vascular connection between the pulmonary artery and the aorta. During the fetal period in the womb, it serves as a bypass circuit for the lungs, which are not supplied with blood. A few days after birth, this connection usually closes automatically to form a cord of connective tissue. After birth, the isthmus usually expands to the normal diameter of the aorta. In ISTA, however, this widening of the isthmus does not occur.
In the most common cases, the narrowing is located before the opening of the ductus (preductal ISTA) and only extends over a few millimeters. In some cases, it can also be located at the level of the duct (juxtaductal ISTA) or after the duct (postductal ISTA). Furthermore, the narrowing may be longer and, as mentioned above, may be accompanied by other malformations (complex form).
Physiology and hemodynamics
Due to the narrowing in the area of the isthmus, there is reduced blood flow in the lower half of the body on the one hand and high blood pressure in the area of the head and upper extremities on the other. The blood ejected from the left heart accumulates in front of the constriction, resulting in a pressure load on the left ventricle.
The extent of the symptoms depends on the severity of the stenosis. In the case of very severe stenosis (critical ISTA of the newborn), the first symptoms become noticeable just a few days after birth, including difficulty drinking, listlessness and possibly life-threatening shock. With less critical constrictions, symptoms may not become noticeable until later in life (infantile form of ISTA) or only in adulthood (adult form of ISTA). The consequences of high blood pressure in the upper half of the body and the pressure load on the left ventricle are in the foreground. The high blood pressure can lead to increased headaches, frequent nosebleeds, cold legs and muscle pain and cramps when walking.
The pressure load on the left ventricle can manifest itself in a general pumping weakness of the heart (heart failure). If ISTA remains undetected, arterial bypass circuits develop in the area of the thoracic and abdominal aorta. On physical examination, the most noticeable signs are weakened or absent pulses in the groin and feet and a difference in blood pressure between the arms and legs. A loud heart murmur can be heard between the shoulder blades.
Treatment of aortic coarctation
Conservative
Permanent conservative treatment of ISTA does not make sense, as it does not eliminate the cause, so that surgical or interventional therapy measures are almost always carried out.
Critical ISTA of the newborn represents an emergency situation due to the frequently occurring shock states, in which stabilization can usually be achieved initially with conservative measures. An initial measure is to keep the slowly closing botallic duct open with medication. This allows the blood supply to the lower half of the body through the pulmonary artery to be maintained for the time being.
In the case of very severe narrowing or prolonged ISTA, a pumping weakness of the left ventricle often develops. This is noticeable in children through reduced physical resilience, accelerated breathing, excessive sweating and failure to thrive. As a rule, therapy with flushing out and heart-protective medication is then necessary.
If ISTA persists for a longer period of time, high blood pressure often develops, which must be treated with medication even after ISTA therapy.
Surgery and intervention
Surgical correction of ISTA is usually possible on the beating heart and without the use of a heart-lung machine. Only complex forms or additional malformations occasionally require surgery using a heart-lung machine. In addition or as an alternative, cardiac catheterization can be used to widen the narrowing with the help of a balloon (balloon dilatation) and insert a stent (stent implantation). These procedures are used in patients with suitable anatomy or if surgery is not possible due to accompanying circumstances. They are also the treatment of choice for the treatment of new constrictions following previous surgery.
Prognosis of aortic coarctation
Further course
Surgical and interventional correction of ISTA are now standard procedures. The chances of success are very good. The postoperative course is generally uncomplicated. However, elevated high blood pressure values often persist, which require drug therapy.
Furthermore, there is a residual risk of a renewed narrowing in the area of the isthmus. Nevertheless, after successful correction, life expectancy is comparable to that of the normal population and everyday life is usually possible without restrictions.
