Description
This combination of four (gr. tetra: four) defects is named after the physician Fallot.
At 6%, tetralogy of Fallot (ToF) is one of the most common congenital heart defects and belongs to the group of cyanotic vitias in which the blood of the systemic and pulmonary circulation is mixed, resulting in a bluish skin coloration.
ToF occurs more frequently with genetic anomalies (DiGeorge syndrome) and can be accompanied by other cardiac anomalies (right aortic arch).
Anatomy
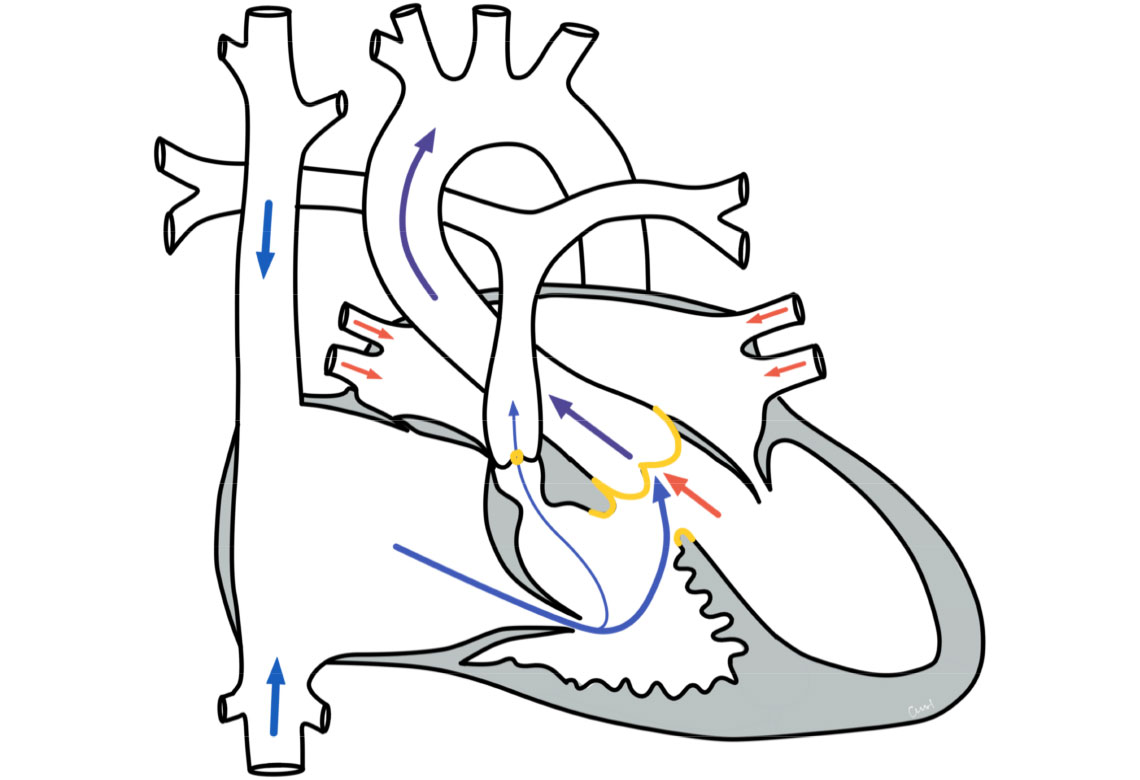
There is a combination of four defects:
- a narrowing of the pulmonary artery valve (pulmonary valve, the narrowing is then called pulmonary stenosis), usually combined with a small pulmonary artery and a narrowing of the outflow tract of the right ventricle below it (due to muscle thickening, right ventricular outflow tract obstruction (RVOTO))
- a thickening of the right ventricle (RV hypertrophy)
- a gap in the thin (membranous) part of the ventricular septum (ventricular septal defect, VSD)
- an "overriding" aorta: The aorta normally originates from the left ventricle. In ToF, it "rides" over the ventricular septal defect and is thus connected to the right and left ventricle.
Physiology and hemodynamics
Due to the ventricular septal defect with the aorta "riding" over it, there is an admixture of non-oxygenated, blue blood from the right half of the heart into the body's circulation. The body is thus supplied with blood with a lower oxygen content, which causes cyanosis (bluish coloration of the skin).
The blue coloration is particularly visible on the tongue, lips, tips of fingers and toes. The more severe the constriction of the right outflow tract and the pulmonary valve, the more pronounced the development of cyanosis.
Excitement in affected children can lead to so-called hypoxic seizures. The build-up of pressure in the chest (often caused by crying or squeezing) and the release of stress hormones exacerbate the already existing constrictions from the right ventricle to the pulmonary circulation and make it even more difficult for blood to flow into the lungs. The blood is therefore less able to be "loaded" (saturated) with oxygen. As a result, the proportion of deoxygenated blood in the body is temporarily higher, which leads to an increase in cyanosis. Cyanosis also often becomes more pronounced during physical exertion.
Therapy of a tetralogy of Fallot
Surgical and interventional therapy
The aim of the therapy is to correct the heart defect. This is only possible through surgery. The operation is usually performed at the age of 6-9 months and must be carried out with the aid of a heart-lung machine. Firstly, the ventricular septal defect is closed with a tissue patch. Secondly, the narrowing of the pulmonary valve is repaired. If necessary, the pulmonary artery is widened with a piece of tissue (patch) and the narrowing of the legal outflow tract is repaired by resecting excess muscle tissue.
Depending on how well the pulmonary valve functions after the procedure, further measures may be necessary. A valve replacement is often necessary years later, in which the pulmonary valve is replaced with another valve (e.g. a tissue-processed valve). If the anatomy is suitable, this is now also possible using a cardiac catheter procedure (percutaneous valve implantation).
If there are additional narrowings in the pulmonary arteries, further cardiac catheter examinations may be necessary in the course of the patient's life in order to widen these narrowings using a balloon catheter or to provide them with a stent.
Initial palliation (stabilization, relief)
If there is a very severe narrowing in the area of the pulmonary valve, surgery or intervention may be necessary early on in the first few weeks of life to ensure the blood supply to the lungs. For this purpose, the pulmonary valve can be widened using a balloon during a cardiac catheterization. In rare cases, this measure cannot be used successfully. If an early correction cannot be carried out, palliation can be used to surgically ensure blood flow to the lungs with a vascular prosthesis (shunt). This involves creating a connection between a large arterial vessel and the pulmonary artery. With these measures, sufficient blood flow to the lungs can be achieved temporarily and the final surgical correction can take place at a later age. Both procedures can be performed on a beating heart and are therefore not dependent on the use of a heart-lung machine.
Prognosis of a tetralogy of Fallot
Further course
Surgical correction of ToF has been around since 1944 and is one of the standardized surgical procedures. The chances of success are very good. The postoperative course is generally uncomplicated. Depending on the severity of the congenital defects, leaks in the area of the pulmonary valve or a residual stenosis in the area of the pulmonary artery may remain after the operation. These findings are often insignificant, but larger residual defects may require treatment later on. For some patients, further operations are therefore necessary in the course of their lives.
After successful correction, life expectancy is comparable to that of the normal population, and patients should be able to go about their daily lives without restrictions, although they may be limited in their ability to exercise.
