MRI interventions
Ultrasound and computed tomography (CT) have proven to be accurate, safe and reliable methods of image support for planning, performing and monitoring minimally invasive interventions. In recent years, however, magnetic resonance imaging (MRI) has become increasingly important due to recent technical developments, as it has considerable advantages over the other methods.
MRI interventions
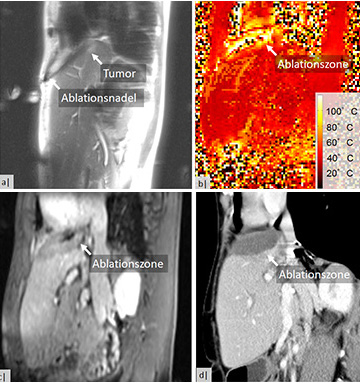
Unlike ultrasound and CT, MRI can visualize lesions that cannot be detected by other means due to its excellent soft tissue contrast. Furthermore, the temperature can be measured with MRI, which is extremely helpful in the context of tumor ablation, as the safety margin around the tumor can be detected. In addition, unlike CT, MRI works without ionizing radiation. The arbitrary positioning and recording of 2D planes and 3D volumes in space enables the image-supported implementation of angulated intervention paths in real time. With the appropriate technology, it is also possible to change the layer planes interactively. This means that even tumors that are difficult to locate and difficult to access, such as lesions in the liver dome near the diaphragm, can be punctured while breathing freely. MRI-guided intervention can thus reduce mortality, lower recurrence rates are possible and the hospital stay can be shortened compared to surgery, particularly in the case of tumor ablation.
For these reasons, interventional MRI (iMRI) is a research focus at our Institute and is also used in patient care. In addition to diagnostic biopsies (e.g. in the liver, kidneys or extremities), we perform minimally invasive cortisone and Botox injections and microwave ablations.
During ablation, pencil-lead-thin applicators are positioned minimally invasively in the tumor to be treated with the help of real-time MRI imaging (see Figure 1). The tissue is then heated locally to up to 120°C, causing the tumor cells to die. We monitor this process using an MRI procedure to record temperatures. Subsequently, two months after the ablation and every six months thereafter, control images are taken to check the success of the treatment and to detect any new tumors at an early stage (see Figure 2).
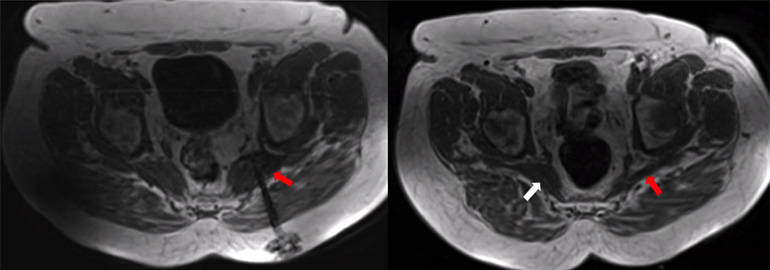
The piriformis muscle is a gluteal muscle that can exert pressure on the immediately adjacent ischiadicus nerve due to various causes such as muscular tension or shortening. This results in a bottleneck syndrome, which manifests itself in the typical sciatica symptoms with pain radiating into the buttocks and leg.
In severe, chronic cases, the MRI-guided injection of botulinum toxin A (Botox®) into the piriformis muscle is a minimally invasive, image-guided treatment option. The neurotoxin prevents the transmission of signals from nerves to the muscle, resulting in temporary denervation and weakening of the muscle. Pain relief is already achieved by the reduced muscle tone; in addition, the smaller volume of the muscle belly relieves pressure on the neighboring sciatic nerve and eliminates the bottleneck. The advantage of MRI-guided puncture is that we can see both the needle and the muscle in the MRI and can therefore inject the botulinum toxin very precisely into the affected muscle (see Figure 1). This significantly increases safety and effectiveness. In addition, the painful sciatic nerve can be temporarily anaesthetized in its course directly below the piriformis muscle (in the infrapiriform foramen) by injecting long-acting local anaesthetics and corticosteroids. This is often useful to break through the acute pain.
At the Institute of Diagnostic and Interventional Radiology, this procedure is used clinically as well as being improved and evaluated as part of scientific projects. We work closely with the Clinical Department for Rehabilitation Medicine at the MHH, which thoroughly examines all patients and rules out other causes of pain.
Prof. Wacker, the Director of the Institute of Diagnostic and Interventional Radiology at the MHH, is one of the pioneers in the field of interventional MRI. Since 1996, he has conducted research and projects in the field of interventional MRI, first in Berlin at the FU, then at Case Western University in Cleveland, Ohio and finally at Johns Hopkins University in Baltimore, Maryland. Together with many colleagues and employees of the Institute, a total of 10 patents and patent applications have been filed and a large number of publications and review articles on this topic have been produced.
Due to this expertise, the MHH is the clinical partner in the STIMULATE research campus, which is one of only 10 initiatives funded in the "Research Campus - Public-Private Partnership for Innovation" program of the Federal Ministry of Education and Research (BMBF)(forschungscampus-stimulate).
One goal of the STIMULATE research campus in the first phase is to establish routine, complete minimally invasive treatment (ablation) of tumors and metastases of the abdomen, in particular the liver, in standard MRI devices(https://youtu.be).
An important research aspect for us in this context is the MRI method used to record temperatures (thermometry) for therapy monitoring in order to guarantee total destruction of the tumor (A0 ablation) while simultaneously protecting the surrounding tissue. Furthermore, we are working together with the engineers and physicists on improving the ablation devices and on instrument tracking in order to transfer the previous intervention approach into an interactive freehand technique. The aim is to enable intuitive layer tracking similar to the handling of ultrasound.
In addition to the collaboration with the physicists and engineers at OvGU Magdeburg, the scientists at MHH have active international collaborations with Johns Hopkins University and the University of Utah.
Doctorate
We offer the possibility of a doctorate for physicists or medical students.
Interested students have the opportunity to work with us as research assistants in this field.
If you are interested, please contact Bennet Hensen hensen.bennet@mh-hannover.de
Hannover Medical School
Institute of Diagnostic and Interventional Radiology
Director: Prof. Dr. med. F. Wacker
Office: Phone +49 (511) 532 3421
Contact iMRT Clinical Department: Dr. med. B. Hensen
Contact person MRI-guided piriformis injection: Dr. med. L. Sonnow
Cooperation partner: Jan Fritz M.D. Johns Hopkins Hospital
Contact person iMRI research: Dr. rer. nat. Marcel Gutberlet