Interventional radiology
Interventional radiology specializes in diagnostic imaging and image-guided therapy, for example for vascular diseases, inflammation, tumours and pain.
While the much better known diagnostic radiology uses imaging procedures to provide important information for diagnosis and to assess the progression of diseases, the field of interventional radiology uses image information for image-guided therapy.
Interventional radiological treatments can be used for a wide range of clinical pictures and are generally characterized by less traumatic access routes compared to surgery. These procedures are therefore also classed as minimally invasive procedures.
Depending on the treatment approach, different access routes are chosen. For example, treatment of the vascular system is possible via the arteries or veins. By making a small puncture in easily accessible vessels, e.g. in the groin, the vessels themselves can be treated for vasoconstrictions and also used as a "transit route" on the way to organs - after all, every organ in the human body receives its nourishment from the blood vessels. For example, catheters can be inserted into the liver through the vessels themselves, which are insensitive to pain, in order to treat tumors locally with chemotherapy, to close small vascular branches in the event of bleeding or even to insert entire vascular prostheses into almost all vascular systems via a catheter.
If the target area cannot be easily reached through the vascular system, radiological imaging using CT, MRI or ultrasound provides the necessary information to reach the organ without damaging important surrounding structures.
Interventional radiology is now a standard procedure in many areas and has replaced open surgical interventions.
The majority of vascular constrictions that could previously only be treated by surgically creating artificial vessels (bypasses) are now treated using interventional radiology. Advances in material development have further increased the reliability of these methods in recent years. For example, very small vessels in the lower leg can now be treated. The use of drug-coated balloons to dilate constrictions has further reduced the need for follow-up therapy. In particular, the side effects caused by a large surgical approach can be significantly reduced with minimally invasive/interventional radiological procedures. In many cases, this also means that the patient's hospital stay can be shortened.
Whether an interventional therapy approach is possible can be decided on the basis of preliminary examinations and findings. In many areas, an interdisciplinary meeting is held to discuss the ideal treatment approach together with vascular surgeons.
Most interventions are performed with image guidance. Where possible, this image guidance is ensured using procedures such as sonography without X-rays, e.g. for vascular punctures, puncturing space-occupying lesions or inserting drains to treat inflammation. If X-rays are used, this is done according to the ALARA principle (As Low As Reasonably Achievable). This means that every effort is made to use as little radiation as possible, but as much as is necessary for the treatment. The radiation exposure for most interventions is slightly higher than the values for computer tomography.
Further information about the Interventional Radiology competence team
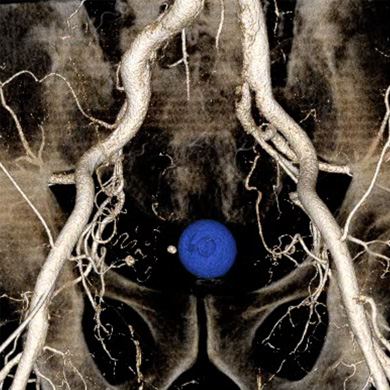
- PROSTATE ARTERY EMBOLIZATION. Minimally invasive procedure for the treatment of urinary tract obstruction caused by benign prostatic hyperplasia.
- VENOUS ACCESSES (ports, tunnel catheters)
- MRT FUSION-ASSISTED ULTRASOUND-GUIDED PROSTATE BIOPSY
- MRI INTERVENTIONS

- PERCUTANE TUMOR ABLATION Minimally invasive , image-guided procedure for the treatment of tumors, especially of the liver, kidneys, lungs or bone. Various techniques are used, in particular microwave (MWA), radiofrequency (RFA) and cryoablation. The exact choice of procedure depends, among other things, on the characteristics and location of the tumour. Depending on the technique, the tumor is either cooled to temperatures below -120°C or heated to temperatures above 100°C.
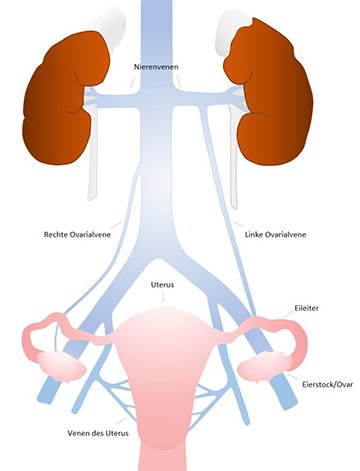
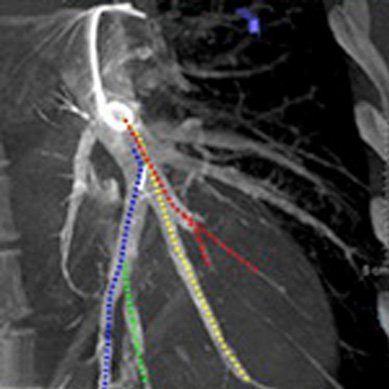
- Pelvic vein sclerotherapy for the minimally invasive treatment of chronic lower abdominal pain due to varicose veins in the pelvis (pelvic vein syndrome, also known as pelvic congestion syndrome).