Pelvic vein sclerotherapy
for the minimally invasive treatment of chronic lower abdominal pain due to varicose veins in the pelvis (pelvic vein syndrome, also known as pelvic congestion syndrome)
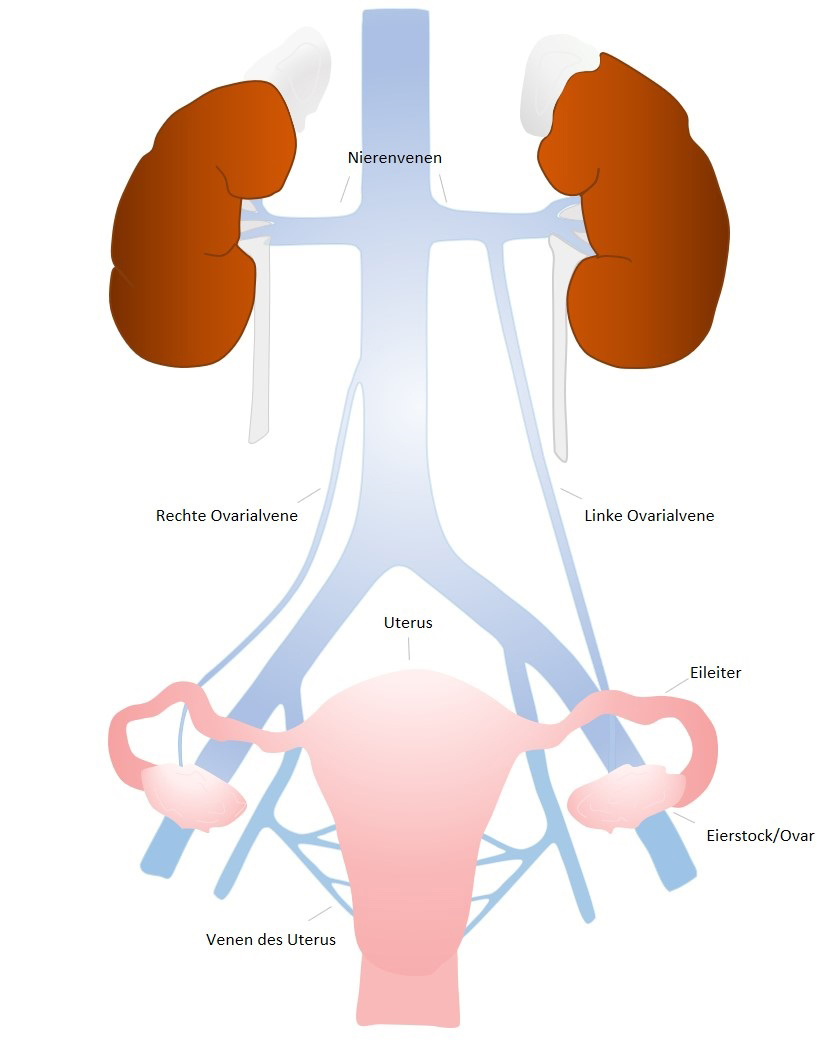
Around 15% of all women between the ages of 18 and 50 suffer from chronic lower abdominal pain (lasting more than 6 weeks). Pelvic congestion syndrome (PCS) is the second most common cause of chronic lower abdominal pain, but in many cases remains undiagnosed1. Young patients in particular are sometimes only diagnosed with pelvic vein syndrome after years of suffering. Pelvic vein syndrome is caused by abnormal dilation of the ovarian and pelvic veins. Veins are blood vessels that carry deoxygenated blood to the heart. If the function of the veins is impaired, blood backs up in the veins and varicose veins develop, which can cause severe discomfort.
Pelvic vein syndrome is typically characterized by chronic pain and a feeling of pressure in the lower abdomen. The symptoms often worsen during long periods of sitting or standing, during or after sexual intercourse, during menstruation or during abdominal straining (e.g. coughing or bowel movements).
Other typical symptoms are
- Back pain, hip pain, groin pain, flank pain
- Visible varicose veins on the mons veneris, labia or legs
- Hemorrhoidal disease, rectal complaints
- Constipation and flatulence
- Problems with urination
Women who have had one or more births belong to the risk group. In addition, congenital deviations from the normal vascular anatomy such as May-Thurner syndrome (compression of the iliac vein by the iliac artery) or nutcracker syndrome (narrowing of the left renal vein by the upper intestinal artery and abdominal aorta) can promote the development of pelvic vein syndrome.

The symptoms caused by pelvic vein syndrome can have a major impact on daily life. Of the treatment options available - e.g. hormone therapy, pain therapy, surgical removal of the uterus and ovaries - minimally invasive sclerotherapy (scerotherapy) of the pelvic veins is the most efficient and least invasive treatment option1.
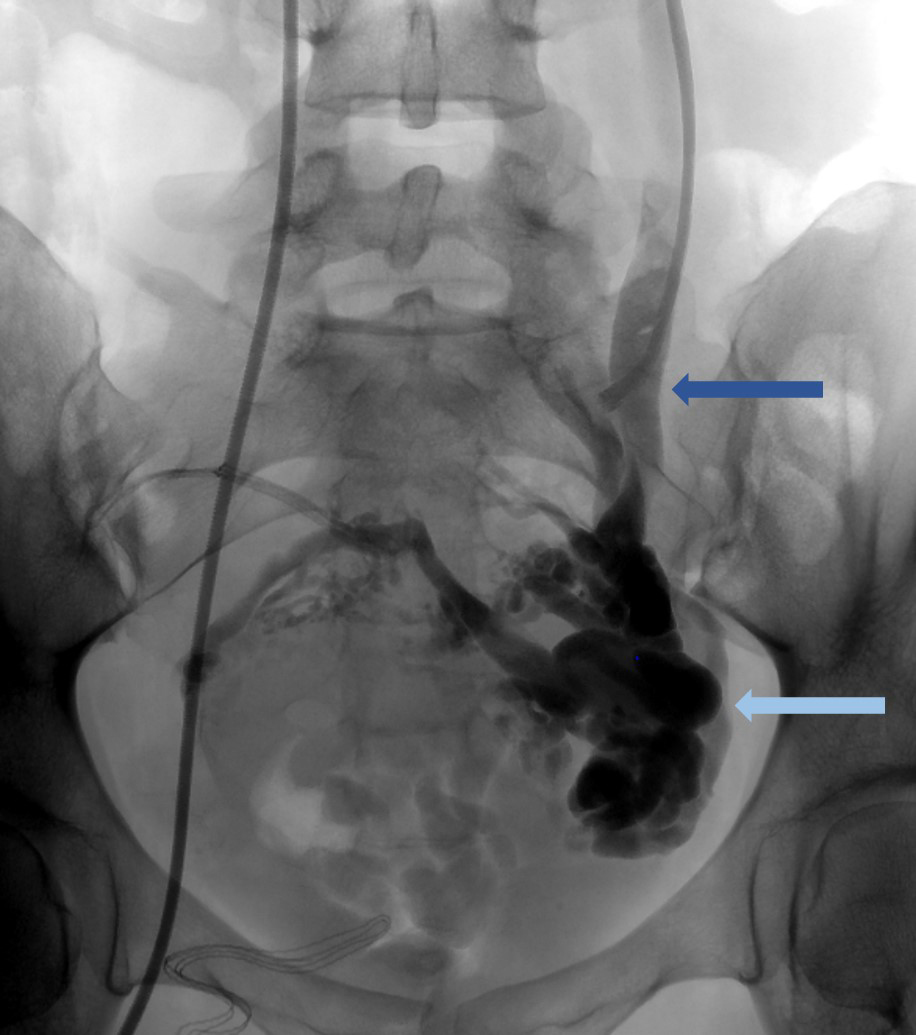
In pelvic vein sclerotherapy, a catheter (= a plastic tube approx. 1 mm in diameter) is inserted into the ovarian vein via a vein in the groin under X-ray control. If the suspicion of a backlog of blood is confirmed here, a foaming sclerosing agent is administered to obliterate the varicose veins. If necessary, additional platinum coils measuring a few millimetres or other gentle closure systems are inserted into the pelvic and ovarian veins to close the varicose veins permanently. This reduces the pressure on the vessels and the above-mentioned symptoms disappear.
The treatment requires a small puncture in the groin, which is performed under local anesthesia. General anesthesia (and the associated risks) is not necessary, so our patients are fully conscious during the entire microtherapeutic procedure. There is generally little or no pain during and after the procedure, so our patients only receive painkillers if necessary.
The procedure usually requires hospitalization for a maximum of 2 nights. Complications during or after pelvic vein sclerotherapy are rare5, the therapy has no negative effects on the menstrual cycle or on fertility2.
The results of this catheter-based treatment for pelvic vein syndrome are promising, with a success rate of over 80%2-4. Our patients are usually symptom-free after one session, with further treatment sessions only being necessary in individual cases.
As we often treat young patients with pelvic vein syndrome, protection from unnecessary X-ray radiation is particularly important to us. At Hannover Medical School, this procedure is therefore supported by the latest generation of angiography equipment.
If a pelvic vein syndrome is suspected, sonography and/or cross-sectional imaging using magnetic resonance imaging (MRI) is performed. In this way, another cause of the lower abdominal pain can be ruled out and the blood vessels in the pelvis can be visualized at the same time. Possible deviations from the normal vascular anatomy can thus be identified before the actual procedure and the examination can be planned accordingly.
If you are interested in this procedure, you can make an appointment in our consultation hours via the Interventional Radiology office. Please bring all previous examination results and any existing CT/MRI examinations of the pelvis (on CD/DVD) with you to this appointment.
1 Meissner M, Gibson K. Clinical outcome after treatment of pelvic congestion syndrome: Sense and nonsense. Phlebology. 2015;30(1_suppl):73-80. doi:10.1177/0268355514568067
2 Kim HS, Malhotra AD, Rowe PC, Lee JM, Venbrux AC. Embolotherapy for Pelvic Congestion Syndrome: Long-term Results. J Vasc Interv Radiol. 2006;17(2, Part 1):289-297. doi:10.1097/01.RVI.0000194870.11980.F8
3 Phillips D, Deipolyi AR, Hesketh RL, Midia M, Oklu R. Pelvic Congestion Syndrome: Etiology of Pain, Diagnosis, and Clinical Management. J Vasc Interv Radiol. 2014;25(5):725-733. doi:10.1016/j.jvir.2014.01.030
4 Antignani P-L, Lazarashvili Z, Monedero JL, et al. Diagnosis and treatment of pelvic congestion syndrome: UIP consensus document. Int Angiol. 2019;38(4):19.
5 Ganeshan A, Upponi S, Hon L-Q, Uthappa MC, Warakaulle Dr., Uberoi R. Chronic Pelvic Pain due to Pelvic Congestion Syndrome: The Role of Diagnostic and Interventional Radiology. Cardiovasc Intervent Radiol. 2007;30(6):1105-1111. doi:10.1007/s00270-007-9160-0