Congenital lobar emphysema
Foreign words:
Congenital - congenital
Lobar - affecting a lobe of the lung
Emphysema - excessive or unusual presence of air
This congenital disease of a lung segment or lobe is caused by a valve mechanism of the malformed bronchus wall. The stabilizing bronchial cartilage is often missing so that air is trapped in a section of the lung after inhalation. This otherwise normal section inflates considerably and compresses the neighboring lung tissue. The upper lobes of the lungs (left more than right) are most frequently affected. The development of the clinical picture depends on functional air breathing, which is why prenatal diagnosis is rare. In about 25% of children, the symptoms are present at birth, in 50% of cases they appear within the first month of life. Diagnosis after the 6th month of life is rare.
In an acute form, children are characterized by shortness of breath, cyanosis (bluish skin color) and retraction of the intercostal muscles. In chronic forms, frequent respiratory infections may be indicative.
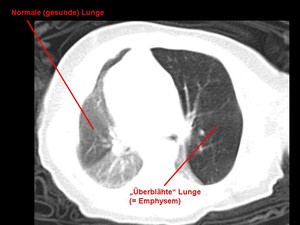
If a congenital malformation of the lungs is suspected, we take an X-ray of the chest (thorax) on the first day of life. A computer tomography (CT) scan of the chest is then carried out. This usually allows the correct diagnosis to be made and other important differential diagnoses (e.g. congenital cystic lung malformation (CCAM) or a pulmonary sequestrum ) to be ruled out.
After this basic diagnosis, the further course of action is then determined, taking into account the clinical condition of the child.
Even if a wait-and-see approach can be adopted in individual cases of very mild forms in the absence of symptoms, most children require surgery Even newborns with symptoms or even children who require artificial respiration can be operated on soon if they are stable. We develop the individual treatment proposal together with our colleagues in pediatric pulmonology (lung medicine).
Minimally invasive surgical technique / Thoracoscopic resection
Depending on the location of the malformation, three or four small incisions (approx. 2-3 mm) are made across the right or left side of the chest during the thoracoscopic (minimally invasive) surgical technique. A thin tube (trocar) is inserted into the chest cavity through each of these incisions. Air is also blown into the chest cavity through one of these trocars and a camera is inserted (thoracoscopy). This allows the affected unilateral chest to be inspected. The remaining trocars are used to insert small working instruments that are needed to remove the malformation. The extent of the resection depends on the size of the findings and ranges from an atypical partial resection to removal of the affected lung lobe.
In individual cases, a small drainage tube (so-called thoracic drainage or pleural drainage) is placed in the pleural cavity (the space between the lung surface and the pleura) in order to maintain or restore the physiological negative pressure. Sometimes a controlled suction is also applied, which serves to pump wound secretions or air out of the pleural cavity. However, this drainage is usually removed again soon after the operation.
Not all children can undergo minimally invasive surgery. Factors such as birth weight, the extent of the lung malformation, other illnesses (such as heart defects) and, above all, the urgency of the treatment all play a role here. The pediatric surgeon may also have to switch to an open surgical technique for technical reasons, for example if the overview during thoracoscopy is inadequate.
Open surgical technique
The main difference between the open surgical technique and the minimally invasive technique is the type of access to the surgical site. Instead of three or four small incisions, a single, longer incision is made over the respective intercostal space - depending on the location of the lung malformation - to provide access to the part of the lung to be resected. With this technique, it may also be necessary to insert a temporary chest drain, which is removed during the inpatient stay.
We always use absorbable suture material. Therefore, no suture removal is necessary after the operation. Scarring depends on the individual's disposition.
By the age of three, lost lung tissue is partially regenerated, resulting in a normal capacity for work and sport, and well over 90% of children develop normal lung function. The long-term results are therefore excellent.
Patients with congenital lobar emphysema must remain in hospital for a few days to weeks after the operation (depending on birth weight and concomitant illnesses). During this period, the child and mother are cared for by our pediatric nurses and the medical team on the infant ward.
3 months after removal of the affected lung section, the child will be seen again by the surgeon in our pediatric surgery outpatient clinic. Here we carry out both a clinical and a radiological (chest X-ray) follow-up.