Interdisciplinary consultations
An amputation, the loss of one or even several body parts, is a drastic life event.
Synchronized, optimal medical, rehabilitative and orthopaedic care is essential for smooth rehabilitation. This is why we established an interdisciplinary amputation consultation in 2021.
Our team consists of plastic surgeons, trauma surgeons, orthopaedic technicians, rehabilitation physicians, pain physicians, neurologists, specialized physiotherapists and occupational therapists. Interdisciplinary cooperation enables us to assess your complaints from different perspectives and formulate and address a joint treatment concept.
With the optimal surgery and structured aftercare, we aim to help our patients return to a more active life.
During our consultations, we discuss your problems with you in order to find the best treatment path for you.
Not only the meticulous examination, but also the subsequent patient-oriented rehabilitation with a broad-based team of experts is crucial!
You are invited to attend the consultation together with your orthopaedic technician. If this is not possible, we will be happy to arrange a video conference with your local provider.
Pimp my Stump 2.0 - Examination and therapeutic procedures
Surgical amputation revisions can be an effective solution for problems associated with amputations that make everyday life with a prosthesis more difficult. Various procedures such as residual limb reshaping, soft tissue reduction, re-amputation, smoothing of painful bone edges, refixation of the soft tissue mantle and nerve realignment can be used.
Our aim is to perform these surgical corrective procedures in a bionic manner. By using innovative amputation techniques, nerves and muscles in the residual limb can be "made functional again" to facilitate interaction with the prosthesis.
"Bionics" means using natural processes and phenomena in nature to solve technical problems and develop innovative, sustainable and resource-saving solutions. In surgery, we modify the human body through surgical interventions in such a way that it can be connected to and communicate with the available technology in the best possible way.
Innovative surgical techniques
TMR is a treatment method developed in Chicago in the early 2000s by Todd Kuiken (rehabilitation physician) and Gregory Dumanian (plastic surgeon) to improve prosthesis control. In a complex microsurgical procedure, a selected severed nerve in the amputation stump is redirected to biomechanically no longer relevant muscles in the socket or near the socket and reinnervates them. This creates a new and additional "myosignal" that can be used to control the prosthesis.
This also reduces the likelihood of painful neuromas developing (again), as the growth of the sprouting nerve fibres is organized and no longer uncontrolled.
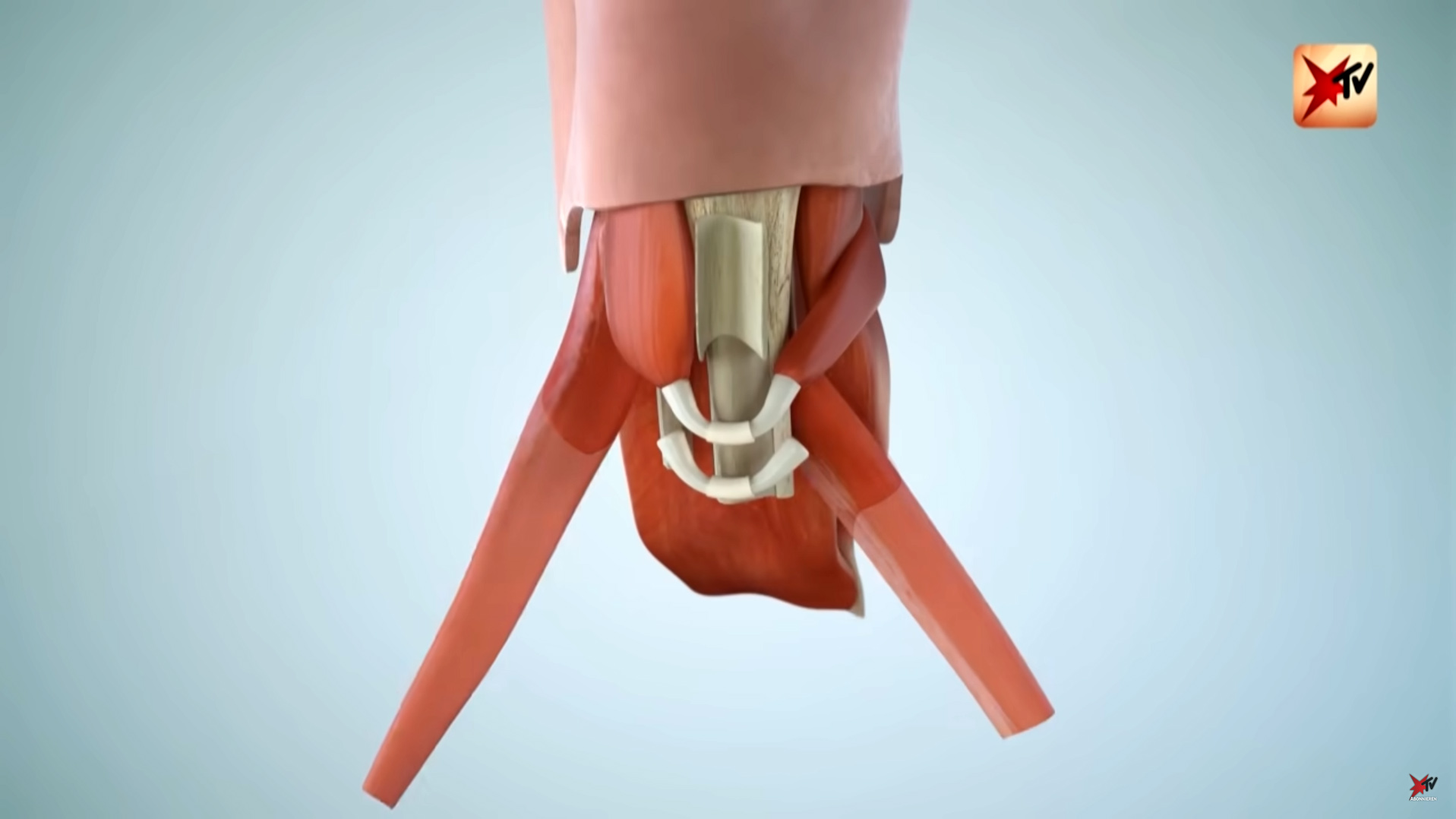
The same principle applies to RPNIs (see animation below). Here, however, the nerve is only embedded in a small, previously resected piece of muscle and sunk into the stump. The organized sprouting and increased function can reduce phantom and neuroma pain.
Sensory feedback on the residual limb in particular is considered crucial for improving prosthetic control, reducing phantom pain and improving embodiment (body awareness).
TSR surgery can be performed to improve this sensory feedback.
The details of the surgical technique depend on the amputation level, as this determines which nerves and skin areas are available for the targeted reinnervation of the skin.
We perform the so-called agonist-antagonist myoneuronal interface technique (AMI) for the majority of primary amputations. Here, muscles - namely the agonists (players) and antagonists (opponents) - are specifically connected to each other. This preserves the original flexion movement as with intact muscles. The aim of the developers from Boston was to restore proprioception. Proprioception describes a person's ability to perceive the position and movement of their body in space even when their eyes are closed. This is also referred to as a "6th sense". This procedure increases the gait and grip stability and safety of those affected.
At the same time, the transposition of the muscles improves the cushioning of the residual limb. The AMI technique is a reinterpretation of myodesis/myoplasty.
The AMI procedure is usually combined with one of the nerve interventions described above.
An osseointegrated prosthesis is a bone-guided prosthesis. An implant is surgically anchored into the bone of the arm or leg stump with part of the implant sticking out via a skin/soft tissue passage - the prosthesis can be docked directly onto this. Problems associated with the socket, such as pressure points and skin problems, no longer occur.
OI is only suitable for certain patients.
We will be happy to advise you in our consultation as to whether you are also suitable for OI.
for AMI patients
Movement exercises for AMI patients
Donations for the AG Innovative Amputation Medicine
If you would like to support our working group and projects, we would be very pleased to receive a donation of your choice. Please use "AG Innovative Amputation Medicine" as the intended purpose.
Companies can also support our work with additional transparency declarations.
The transfer should be made to the following account:
Förderstiftung MHH plus
Sparkasse Hannover
IBAN: DE95 2505 0180 0900 4444 44
BIC: SPKHDE2HXXX
Purpose: AG Innovative Amputation Medicine
Please remember to include your address details when making a bank transfer so that we can issue you with a donation receipt.
Thank you very much for your support!
the Innovative Amputation Medicine Working Group at NIFE
Lower Saxony Centre for Biomedical Engineering, Implant Research and Development
Important information
For a differentiated consultation, please bring the following documents with you to your appointment:
- Referral from a specialist in surgery, trauma surgery or orthopaedics "Specialist consultation in amputation medicine"
- Previous imaging (X-ray/CT/MRI) on a CD-ROM in DICOM format incl. written findings
- Reports from previous treatments (e.g. surgical reports)
- Prosthesis model, socket model
- Current medication plan