Radical cystectomy for bladder cancer
For the treatment of muscle-invasive, i.e. locally advanced carcinomas, we offer the complete spectrum of maximum surgical care. If a cystectomy (removal of the entire bladder) is necessary, we aim to create an orthotopic replacement bladder for cosmetic and functional reasons, if possible. The MHH also has outstanding expertise in the field of bladder replacement. If the local situation allows, a nerve-sparing procedure is performed to improve postoperative continence (and in men to preserve potency).
Instructions for the immediate post-operative phase:
After the operation, you will be taken back to our urology ward. In exceptional cases, certain concomitant diseases may require monitoring in the intensive care unit. Regular blood samples are taken to check important laboratory values and correct them therapeutically if necessary. Wound healing is monitored during ward rounds and dressing changes. Depending on the type of dressing and wound healing, these are necessary at different frequencies. Body fluids of all kinds (lymph, blood, urine, etc.) are drained from the wound area via the inserted drains, usually two. The drains are removed in the post-operative course on the physician's orders. The diet is built up gradually depending on bowel activity, usually from the second or third postoperative day. Regular and preferably soft bowel movements should be ensured so that the wound area is not strained by unnecessary straining. You may be given medication for this. Usually on the tenth day after the operation, the urinary drainage system is checked using a contrast agent to ensure that the suture between the bladder and urethra is tight. If this is the case, the ureteral stents can be removed.
After hospitalization:
Full baths and saunas are prohibited until the wound is completely closed (approx. 3 - 4 weeks depending on wound healing). You should avoid heavy lifting (loads over 5 kg) and physical exertion for at least 4 weeks. Direct pressure on the perineal region, such as that caused by cycling, should be avoided for at least 3 months. Contact your urologist immediately if you have a fever, a burning sensation when urinating or foul-smelling urine, especially if flank pain is also present. It could be a urinary tract infection (with or without urinary retention) of the kidneys. Regular oncological follow-up care is provided by the urologist in charge.
Common urinary derivatives
The most common urinary diversions are briefly presented here, but must be discussed individually depending on the findings and the previous findings of our patients:
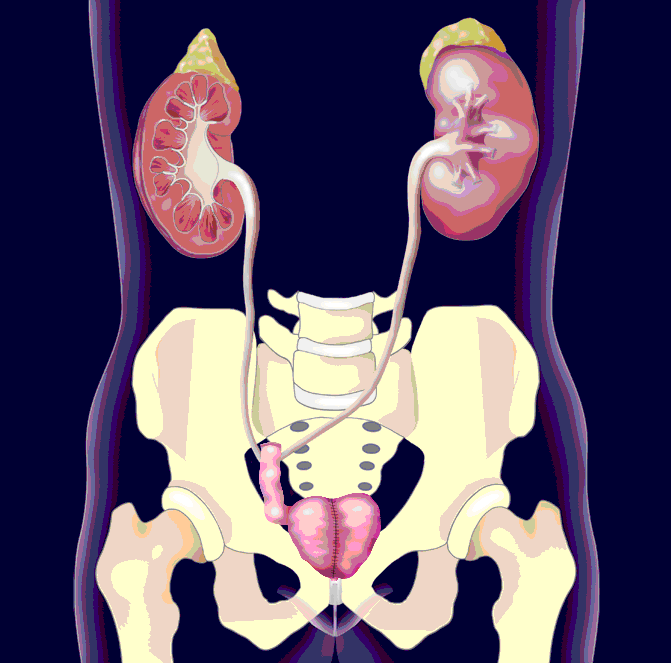
A short segment (approx. 17 cm) is removed from the small intestine, connected to the ureters and drained from the skin. The advantage of this urinary diversion is the quicker procedure with fewer early and late complications. The disadvantage is the incontinent stoma (urine outlet via the skin), which must be supplied with bags.
In this treatment method, a replacement bladder (pouch) made from parts of the small intestine is drained via a stoma. This procedure is suitable for patients in whom the urethra has had to be removed and a continent urinary diversion is desired.
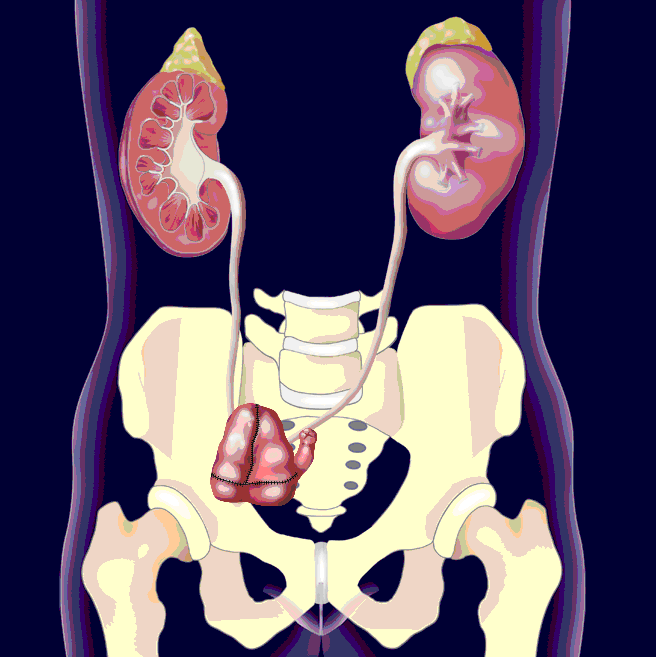
For this purpose, various parts of the intestine cut out of the bowel are sutured together to form a ball and connected to the ureters and urethra. In order to maintain the natural urinary tract, the urethra is then sutured to the bladder again with maximum protection of the external sphincter muscle. A high percentage of patients are continent and pass urine via the urethra as usual.