AG Pediatric Anesthesia
The physiology, homeostasis and also the needs of children under anesthesia differ from those of adults. The underlying diseases that lead to operations and treatments or the indication for anesthesia are also different in pediatrics. We want to continuously improve pediatric anesthesia by increasing the evidence for our actions through research.
Our research in pediatric anesthesia therefore focuses on clinical questions, the results of which are incorporated into guidelines and recommendations or increase the safety of anesthesia.
We participate in international multicenter studies on current issues in paediatric anaesthesia and work closely with our partners in pediatric medicine. We also work on overarching, highly topical issues such as sustainability in anesthesia.
Knowledge for the best treatment of our patients is what drives us.
The individual studies are listed under our focus areas. Students who are interested in a doctorate in pediatric anesthesia are welcome to contact us.
Information on our clinical activities in the field of pediatric anesthesia,
Doctoral students
| Thurgkai Chandrakumar Preoperative shortened fasting times for clear fluids in children | Florian Rahlfs Descriptive analysis of anesthesia in children with congenital heart defects at a supraregional EMAH center |
| Anna Drellmann Adults with congenital heart defects - A descriptive analysis of anesthesiological care at a supraregional EMAH center over a 10-year period | Mike Rosenplänter Influence of intraoperative volume therapy with colloids on hemodynamics, postoperative acid-base status and postoperative recovery |
| Patrick Kuhlmann Elimination of sevoflurane after switching from inhaled to total intravenous anesthesia | Yehor Huzhva Complications and risk factors in anesthesia of children for foreign body aspiration |
| Yevheniia Tkachuk Impact of the liberalization of preoperative fasting requirements in pediatric anesthesia on real fasting times and OR procedures | Sarah Seidel Complications and risk factors in anesthesia and analgosedation of children for PEG/PEJ placement |
| Lisa Vetter Short procedures without infusion therapy in children - results of a prospective multicenter observational study | Alexander Dierkes In vitro characterization of the antimicrobial efficacy of nitric oxide and hydrogen sulfide scavengers against bacteria and fungi and the influence on their sensitivity to (chemo)therapeutics |
| Muriel Wegner Evaluation of the quality of cardiopulmonary resuscitation in the media and comparison with the German resuscitation register using the example of the TV series Grey's Anatomy | Caroline Heckmann Evaluation of aspiration risk, ventilation complications and transfer times in patients with endotracheal tubes vs. supraglottic airway protection during laparoscopic gynecological procedures. |
| Nathalie Weigt Obstetric anesthesia in women with congenital heart defects - retrospective evaluation at a supraregional EMAH center |
Projects
Ongoing studies
Participation in the EUROFAST Study. Data inclusion MHH: 9/22-12/23
The new preoperative fasting guideline of the European Society of Anaesthesiology and Intensive Care (ESAIC, 2022) recommends a minimum fasting time of one hour for clear fluids. This represents a significant change in the practice of pediatric anesthesia. During the transition to shorter fasting times on a global scale, we need a large multicenter audit to monitor the incidence of pulmonary aspiration. The primary aim of the European Preoperative Fasting Audit (EUROFAST) is to determine the safety of reducing the required fasting time for clear fluids to at least one hour in fasting children before elective procedures requiring general anesthesia (as recommended in the ESAIC guideline).
Guideline coordination
S1 Guideline 001-047 "Perioperative fasting times in children and adolescents", Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e. V. (awmf.org). Validity: 3/22-2/27
Completed studies
Dennhardt N, Beck C, Huber D, Sander B, Boehne M, Boethig D, Leffler A, Sümpelmann R. Optimized preoperative fasting times decrease ketone body concentration and stabilize mean arterial blood pressure during induction of anesthesia in children younger than 36 months: a prospective observational cohort study. Paediatr Anaesth. 2016 Aug;26(8):838-43.
Dennhardt N, Beck C, Huber D, Nickel K, Sander B, Witt LH, Boethig D, Sümpelmann R. Impact of preoperative fasting times on blood glucose concentration, ketone bodies and acid-base balance in children younger than 36 months: A prospective observational study. Eur J Anaesthesiol. 2015 Dec;32(12):857-61.
Beck CE, Witt L, Albrecht L, Dennhardt N, Böthig D, Sümpelmann R. Ultrasound assessment of gastric emptying time after a standardized light breakfast in healthy children: A prospective observational study. Eur J Anaesthesiol. 2018 Dec;35(12):937-941.
Beck CE, Witt L, Albrecht L, Winstroth AM, Lange M, Dennhardt N, Boethig D, Sümpelmann R. Ultrasound assessment of gastric emptying time in preterm infants: A prospective observational study. Eur J Anaesthesiol. 2019 Jun;36(6):406-410.
Beck CE, Chandrakumar T, Sümpelmann R, Nickel K, Keil O, Heiderich S, Boethig D, Witt L, Dennhardt N. Ultrasound assessment of gastric emptying time after intake of clear fluids in children scheduled for general anesthesia-A prospective observational study. Paediatr Anaesth. 2020 Dec;30(12):1384-1389. doi: 10.1111/pan.14029.
Beck CE, Rudolp D, Becke-Jakob K, Schindler E, Etspüler A, Trapp A, Fink G, Müller-Lobeck L, Röher K, Genähr A, Eich C, Sümpelmann R. Real fasting times and incidence of pulmonary aspiration in children: Results of a German prospective multicenter observational study. Paediatr Anaesth. 2019 Oct;29(10):1040-1045. doi: 10.1111/pan.13725.
Beck CE, Rudolph D, Mahn C, Etspüler A, Korf M, Lüthke M, Schindler E, Päukert S, Trapp A, Megens JHAM, Oppitz F, Badelt G, Röher K, Genähr A, Fink G, Müller-Lobeck L, Becke-Jakob K, Wermelt JZ, Boethig D, Eich C, Sümpelmann R. Impact of clear fluid fasting on pulmonary aspiration in children undergoing general anesthesia: Results of the German prospective multicenter observational (NiKs) study. Paediatr Anaesth. 2020 Aug;30(8):892-899. doi: 10.1111/pan.13948.
Witt L, Lehmann B, Sümpelmann R, Dennhardt N, Beck CE. Quality-improvement project to reduce actual fasting times for fluids and solids before induction of anaesthesia. BMC Anesthesiol. 2021 Oct 26;21(1):254.
Frykholm P, Disma N, Andersson H, Beck C, Bouvet L, Cercueil E, Elliott E, Hofmann J, Isserman R, Klaucane A, Kuhn F, de Queiroz Siqueira M, Rosen D, Rudolph D, Schmidt AR, Schmitz A, Stocki D, Sümpelmann R, Stricker PA, Thomas M, Veyckemans F, Afshari A. Pre-operative fasting in children: A guideline from the European Society of Anaesthesiology and Intensive Care. Eur J Anaesthesiol. 2022 Jan 1;39(1):4-25.
Malignant hyperthermia is a rare metabolic disorder of the skeletal muscles that is usually triggered by trigger substances (volatile anesthetics or succinylcholine). If the predisposition to malignant hyperthermia is known, the anesthesia machine must first be decontaminated from residual concentrations of volatile anesthetics using an activated carbon filter or flushing method so that the anesthesia can then be performed "trigger-free".
Our working group is primarily concerned with the technical implementation of trigger-free anesthesia in cases of suspected or proven increased risk of malignant hyperthermia. Among other things, we use an ion mobility spectrometer with gas chromatographic pre-separation to detect volatile anesthetics even in very low concentrations.

Ongoing studies
Elimination of sevoflurane after switching from inhalation to total intravenous anesthesia:
Using healthy volunteers (without a predisposition to malignant hyperthermia), the study aims to determine how quickly the sevoflurane concentration can be reduced to < 5 ppm when switching from inhalational to total intravenous anesthesia using activated charcoal filters in inspiratory breath and whether the concentration can be maintained < 5 ppm over a period of 60 min, which is considered a safe threshold for a malignant hyperthermia reaction.
Completed studies
Zumsande S, Thoben C, Dennhardt N, Krauß T, Sümpelmann R, Zimmermann S, Rüffert H, Heiderich S. Rebounds of sevoflurane concentration during simulated trigger-free pediatric and adult anesthesia. BMC Anesthesiol. 2023 Jun 8;23(1):196
Heiderich S, Thoben C, Dennhardt N, Sümpelmann R, Kraus T, Zimmermann S. Preparation of Dräger Atlan A350 and General Electric Healthcare Carestation 650 anesthesia workstations for malignant hyperthermia susceptible patients. BMC Anesthesiol. 2021 Dec 13;21(1):315
Thoben C, Dennhardt N, Krauß T, Sümpelmann R, Zimmermann R, Rüffert H, Heiderich S. Preparation of anaesthesia workstation for triggerfree anaesthesia: An observational laboratory study. Eur J Anaesthesiol. 2019 Nov;36(11):851-856.
Heiderich S, Thoben C, Dennhardt N, Koppert W, Krauß T, Sümpelmann R, Zimmermann S, Klingler W. Low anaesthetic waste gas concentrations in postanaesthesia care unit: A prospective observational study. Eur J Anaesthesiol. 2018 Jul;35(7):534-538
Guidelines
Rüffert H, Bastian B, Bendixen D, Girard T, Heiderich S, Hellblom A, Hopkins PM, Johannsen S, Snoeck MM, Urwyler A, Glahn KPE; European Malignant Hyperthermia Group. Consensus guidelines on perioperative management of malignant hyperthermia suspected or susceptible patients from the European Malignant Hyperthermia Group. Br J Anaesth. 2021 Jan;126(1):120-130.
PhD students
Patrick Kuhlmann
At 4.4%, the healthcare sector is responsible for a high proportion of greenhouse gas emissions in industrialized countries. Greenhouse gases also include anaesthetic gases, of which only a small proportion is metabolized (desflurane 0.02 %, sevoflurane 5 %, isoflurane 0.2 %). A large proportion is discharged directly into the atmosphere via the anesthetic gas transport system (AGFS). In recent years, anesthetic gas absorbers have been developed to collect the gas, e.g. Contrafluran® (Zeosys (Luckenwalde, Germany), The anesthetic gas can be recovered by sterile distillation and reused. This creates a circular economy that saves material and CO2 in the production of anesthetic gases.
Due to the selective release of anesthetic gases into the atmosphere, their short lifespan and the associated low accumulation in the atmosphere, anesthetic gases may have no impact on global warming. Some climate researchers assume that the production, distribution and transportation of the filters for distilling the gas are more likely to lead to additional CO2 emissions that could be relevant to global warming. Nevertheless, their use may make sense, as replacing AGFS with anesthetic gas absorbers would mean savings in energy, maintenance and acquisition costs. However, the anesthetic gas absorber must be so tight that no gas leakage is detectable. We investigated this using an ion mobility spectrometer with gas chromatographic pre-separation in the ppb range for various fresh gas flows.
In the future, the leakage of anesthetic gases will be investigated using different surgical techniques. The use of anesthetic gas absorbers on the heart-lung machine is also of interest.
Ongoing studies
Prospective, multicenter observational study to determine the efficiency of activated charcoal filters and the recovery of sevoflurane used in the operating theatre.
Completed studies
Schultz B, Schultz M, Boehne M, Dennhardt N: EEG monitoring during anesthesia in children aged 0 to 18 months: amplitude-integrated EEG and age effects. BMC Pediatr 2022; 22:156.
Dennhardt N, Arndt S, Beck C, Boethig D, Heiderich S, Schultz B, Sümpelmann R: Effect of age on Narcotrend Index monitoring during sevoflurane anesthesia in children below 2 years of age. Paediatr Anaesth. 2018; 28: 112-119.
Dennhardt N, Beck C, Boethig D, Heiderich S, Horke A, Tiedge S, Boehne M, Sümpelmann R: Impact of temperature on the Narcotrend Index during hypothermic cardiopulmonary bypass in children with sevoflurane anesthesia. Perfusion. 2018; 33: 303-309.
H Köditz, A Drouche, N Dennhardt, M Schmidt, M Schultz, Barbara Schultz: Depth of anesthesia, temperature, and postoperative delirium in children and adolescents undergoing cardiac surgery. BMC Anesthesiol. 2023 May 2;23(1):148. doi: 10.1186/s12871-023-02102-3.
Heiderich S, Ghasemi T, Dennhardt N, Sümpelmann R, Rigterink V, Nickel K, Keil O, Böthig D, Beck CE: Correlation of exhaled propofol with Narcotrend index and calculated propofol plasma levels in children undergoing surgery under total intravenous anesthesia - an observational study. BMC Anesthsiol 2021; 21: 161.
Dennhardt N, Boethig D, Beck C, Heiderich S, Boehne M, Leffler A, Schultz B, Sümpelmann R: Optimization of initial propofol bolus dose for EEG Narcotrend Index-guided transition from sevoflurane induction to intravenous anesthesia in children. Paediatr Anaesth. 2017; 27: 425-432.
Ongoing studies
Observational study on current transfusion practicein children (TRAPA study)
Multicenter, international, German-language, prospective observational study on current transfusion practice and triggering transfusion triggers in children from birth to < 18 years in the context of surgical procedures, interventions, neonatal or intensive medical care or in the intensive care unit (TRAPA study)
Current principles: Transfusion indications in neonates, children and young adults under 18 years of age: The decision to transfuse should be made in consideration of evidence- or consensus-based guidelines. Univ.-Prof. Dr. Steinbicker, together with Priv.-Doz. Dr. Eva Wittenmeier from Mainz and Priv.-Doz. Dr. Florian Piekarski from Frankfurt, wrote a review on the current evidence of transfusion practices in children. It has currently been submitted to the German Medical Journal. The initiators of the University Hospital Frankfurt have already published the following article on the changes in transfusion strategies for erythrocyte units: Changes in Transfusion Practice in Children and Adolescents over Time. Piekarski F, Steinbicker A, Zacharowski K, Meybohm P. Transfus Med Hemother. 2020 Oct;47(5):379-384. doi: 10.1159/000511231. Epub 2020 Sep 16.
The evidence for transfusion in neonates, children and young adults under 18 years of age is unfortunately very limited. For the blood products fresh frozen plasma, platelets and coagulation products fibrinogen, PPSB, antithrombin III, etc., there is currently even less evidence regarding transfusion practice in children under 18 years of age than for red blood cell concentrates. Because there is little evidence, the guidelines are sometimes divergent and often characterized by expert opinions. The studies that are available have a low number of cases, are not prospective in nature and are determined by current clinical practice. Clinical practice, in turn, is very different in the individual centers. In order to make an important contribution to the scientific assessment of transfusion practice in children, we hereby apply for a multicentre, international, prospective observational study by means of an anonymized survey of transfusion practice from the individual centers.
The prospective observational study will address the following objectives:
Prospective survey
- the practiced transfusion triggers
- the transfusion times
- the influence of transfusion on the administration of catecholamines
- the indication for the administration of ECs, FFPs, TCs, fibrinogen and PPSB
- the administration of FFP as volume replacement the administration of TC prophylactically and for the treatment of bleeding
- the proportion of baby ECs
- the proportion of irradiated ECs
in children under 18 years of age in the perioperative, interventional or intensive care setting.
Study coordinators
PD. Dr. Christiane Beck, Dr. Vanessa Rigterink, Dr. Astrid Wintering and Dr. Carolin Böhne in cooperation with Prof. Dr. Andrea Steinbicker, Cologne and PD. Dr. Eva Wittenmeier
Publications
Dennhardt N, Sümpelmann R, Horke A, Keil O, Nickel K, Heiderich S, Boethig D, Beck CE: Prevention of postoperative bleeding after complex pediatric cardiac surgery by early administration of fibrinogen, prothrombin complex and platelets: a prospective observational study. BMC Anesthesiol 2020; 30: 1384-1389.
Perioperative infusion therapy is an essential component in maintaining homeostasis in children. Application studies on the safety of crystalloid and colloidal infusion solutions have contributed significantly to the S1 guideline "Perioperative infusion therapy in children". In addition to studies on osmolality, we also deal with the physical compatibility of drugs with infusion solutions. Intravenously administered drugs frequently used in anaesthesiology have been tested with acetate-containing balanced whole electrolyte solutions, colloidal infusion solutions and the stability of balanced whole electrolyte solutions after the addition of glucose. We are currently testing the physical stability of ibuprofen and paracetamol ready-to-use infusion solutions with various anesthetic drugs.
Ongoing studies
Physical stability of ibuprofen and paracetamol prefusion solution with various anesthetic drugs.
Former PhD students
Dr. Jonas Jürgens
Dr. Anna Auf der Springe
Completed studies
Tscharntke L, Sümpelmann R, Rudolph D, Röher K, Vetter M, Boethig D, Eich C, Dennhardt N: Short anaesthesias without intravenous fluid therapy in children (KEINS): Results of a prospective non-interventional multicenter observational study. Paediatr Anaesth 2024; 34:454-458.
Rudolf D, Witt L, Boethig D, Rigterink V, Zander R, Dennhardt N: The impact of modified fluid gelatin 4% in a balanced electrolyte solution on plasma osmolality in children - A noninterventional observational study. Paediatr Anaesth. 2022; 32: 961-966.
Sümpelmann R, Camporesi A, Galvez I, Pechilkov D, Eich C, Kretz FJ, Perera Sarri R, Tancheva D, Serrano-Casabon S, Murphy P, Astuto M, Zanaboni C, Becke K, Dennhardt N: Modified fluid gelatin 4% for perioperative volume replacement in pediatric patients (GPS): Results of a European prospective noninterventional multicenter study. Paediatr Anaesth 2022; 32: 825-833.
Heiderich S, Dennhardt N, Hartmann H, Kluger GJ, Sümpelmann R, Herberhold T: Stability of 0.5% Glucose-Containing Balanced Electrolyte Solutions for Patients on Ketogenic Diets: A Laboratory Study. Neuropediatrics 2020; 51: 397-400.
Heiderich S, auf der Springe A.,Jürgens J, Koppert W, Leffler A, Sümpelmann R, Dennhardt N: Compatibility of common IV drugs with 6% hydroxyethyl starch 130/0.42 and 4% gelatin. Paediatr Anaesth. 2018; 28: 87-93.
Heiderich S, Jürgens J, Rudolf D, Dennhardt N, Echtermeyer F, Leffler A, Sümpelmann R, Lichtinghagen R, Witt L: Compatibility of common drugs with acetate-containing balanced electrolyte solutions in pediatric anesthesia. Paediatr Anaesth. 2016; 26: 590-598.
Witt L, Glage S, Lichtinghagen R, Pape L, Boethig D, Dennhardt N, Heiderich S, Leffler A, Sümpelmann R: Impact of high doses of 6% hydroxyethyl starch 130/0.42 and 4% gelatin on renal function in a pediatric animal model. Paediatr Anaesth. 2016; 26: 259-265.
Sümpelmann R, Mader T, Dennhardt N, Witt L, Eich C, Osthaus WA: A novel isotonic balanced electrolyte solution with 1% glucose for intraoperative fluid therapy in neonates: results of a prospective multicentre observational postauthorization safety study (PASS). Paediatr Anaesth. 2011; 21: 1114-1118.
Dennhardt N, Schoof S, Osthaus WA, Witt L, Bertram H, Sümpelmann R: Alterations of acid-base balance, electrolyte concentrations, and osmolality caused by nonionic hyperosmolar contrast medium during pediatric cardiac catheterization. Paediatr Anaesth. 2011; 21: 1119-1123.
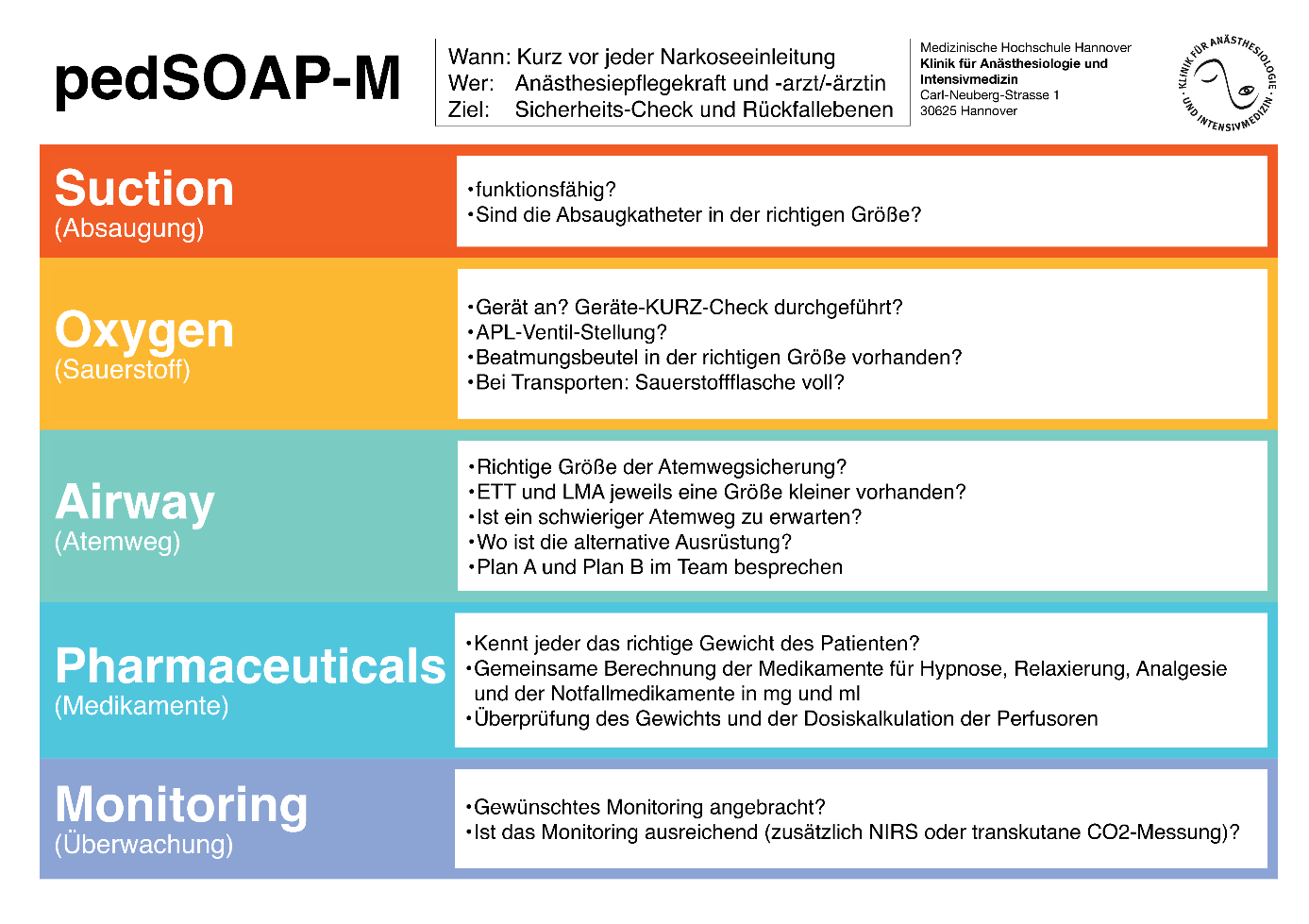
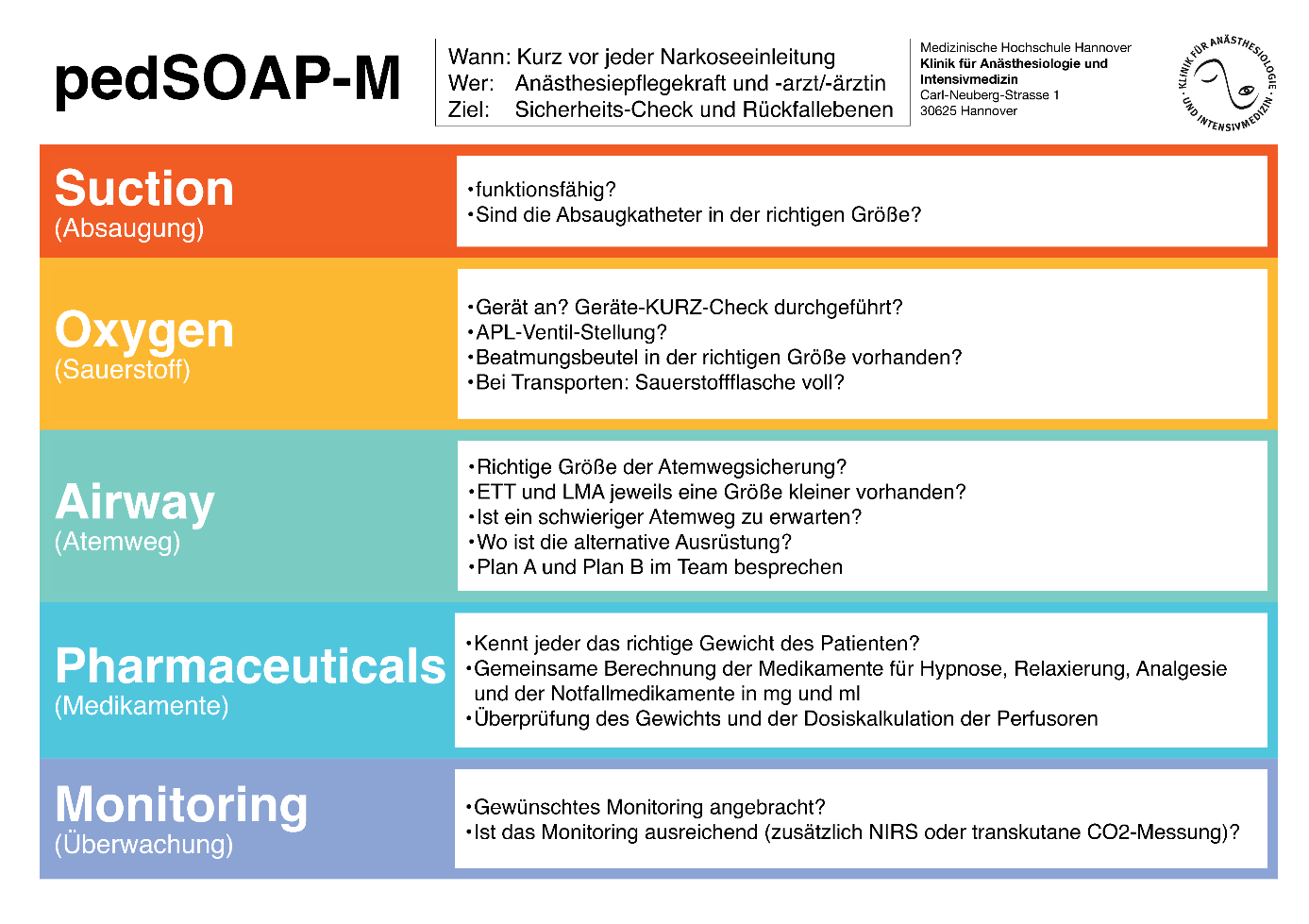
Checklists are playing an increasingly important role in medicine to prevent patient errors. We have heavily modified a checklist published years ago, which was intended for American pediatricians before sedation prior to painful or diagnostic procedures, for our purposes and use it under the synonym pedSOAP-M as a briefing tool. Errors in medicine are often caused by miscommunication. The introduction of the pedSOAP-M promotes Communications in the pediatric anesthesia team and increases the exchange of relevant information. A short briefing lasting 1-2 minutes immediately before induction can reveal potential errors in advance. The "effort to added value correlation" is clearly positive.
Potential impact on patient safety
It is known that avoidable individual errors or the unfortunate concatenation of several errors can lead to patient danger or harm to the patient. It is therefore important to implement a "zero tolerance strategy" for errors in anesthesia in order to prevent unfortunate concatenations. Incorrect doses of medication in particular can quickly become dangerous when patient weights are often very low, as large deviations from the intended dose can occur.
Degree of implementation
Since February 2020, we have implemented briefings in accordance with the pedSOAP-M scheme across the board in the pediatric anesthesia team at Hannover Medical School (MHH). Since then, it has been accepted by all team members and is carried out
Publications
Keil O, Wegener JB, Schiller B, Vetter M, Flentje M, Eismann H. Implementation and adoption of SOAP-M and SBAR at a German anesthesiology department - a single-center survey study. BMC Anesthesiol. 2024 Jul 26;24(1):255. doi: 10.1186/s12871-024-02650-2. PMID: 39060969; PMCID: PMC11282676.
Wegener J, St Pierre M, Keil O, Eismann H. Correlation between safety attitudes and early adoption of cognitive aids in the German culture sphere: a multicenter survey study. BMC Health Serv Res. 2022 Sep 30;22(1):1215. doi: 10.1186/s12913-022-08581-3. PMID: 36175882.
Keil O, Brunsmann K, Boethig D, Dennhardt N, Eismann H, Girke S, Horke A, Nickel K, Rigterink V, Sümpelmann R, Beck CE. Incidence and characteristics of errors detected by a short team briefing in pediatric anesthesia. Paediatr Anaesth. 2022 Oct;32(10):1144-1150. doi: 10.1111/pan.14535. Epub 2022 Jul 31. PMID: 35876723.
Schiller B, Eismann H, Keil O. SOAP-M and SBAR: Concept for improving patient safety in the interprofessional team, in Jahrbuch Intensivmedizin 2020, B. Böttinger and W. Kuckelt, Editors. 2020, Pabst Science Publishers: Lengerich, Germany. p. 279-286.
Brunsmann K, Beck CE, Keil O. Improving patient safety by introducing a structured team briefing immediately before induction of pediatric anesthesia. Pediatric Nurs. 2022. 41(6): p. 163-165
Congress contributions
Keil O, Rigterink V, Nickel K, Eismann H, Horke A, Boethig D, Beck C. Evaluation of a TEAM briefing prior to induction of anesthesia for pediatric cardiac surgery. 52nd Annual International Conference of the DGfK and 15th Focus Conference Heart of the DGTHG and DGfK - Münster, November 3-5, 2023. Cardiotechnology 32 (S1): p 1-77, November 2023. DOI 10.47624/kt.032.KCBU3783
Keil O, Brunsmann K, Dennhardt D, Eismann H, Girke S, Nickel K, Rigterink V, Sümpelmann R, Beck CE. Evaluation of a TEAM briefing prior to induction of pediatric anesthesia. Abstract Annual Congress of the German Society of Anesthesiology and Intensive Care Medicine (DAC 2022). Anesth Intensivmed 2022; 63: S200
Schiller B, Keil O, Koppert W. SBAR and SOAP-M - Implementation in the interprofessional team. 29th Symposium Intensive Medicine and Intensive Care Bremen. Journal of Anesthesia and Intensive Care 2019 (2), 154-157
Prizes and awards
DGTHG Prize Focus Conference Heart 2023, €1,000 for the best lecture, incl. abstract at the 52nd International Annual Conference and 15th Focus Conference Heart from November 3-5, 2023 in Münster of the German Society for Cardiotechnology (DGfK) and the German Society for Thoracic, Cardiac and Vascular Surgery (DGTHG)
German Patient Safety Award 2022, Aktionsbündnis Patientensicherheit e.V., Berlin, 3rd place, €3,500. Keil O, Brunsmann K, Beck C. Improving patient safety by introducing a structured team briefing immediately prior to induction of pediatric anesthesia
LOM-Krankenversorgung 2018, MHH, 1st place, 3.000€, Keil O, Eismann H, Flentje M, Rudolph D, Schiller B, Strackfeldt A, Vetter M, Wiegand, H. Introduction of structured briefings and debriefings to improve quality and increase patient safety in the context of anesthesiology activities.
Ongoing studies
Pediatric surgery
Influence of intraoperative volume therapy with colloids on hemodynamics, postoperative acid-base status and postoperative recovery.
Pediatric pulmonology
Investigation of complication rates during bronchoscopy for foreign body removal by flexible or rigid bronchoscopy.
Pediatric gastroenterology
Anesthesiologic complication rates for PEG procedures in infants compared to older children.
JEMAH
The risk of children with congenital heart defects is also increased during anesthesia for non-cardiac surgery. Many of these children are regularly cared for at the MHH. The anesthesia data of these children from the last 10 years are analyzed with regard to management, complication rates and postoperative course.
Transplantation medicine
The MHH is a center with great expertise in transplantation medicine in children. It is one of the few centers in Europe that also performs lung transplants in infants.
The number of infants for liver transplantation is also high compared to other centers. Anesthesia management is complex and requires a great deal of experience.
The anesthesia data of the last 10 years for all lung and liver transplants in children are evaluated.
Kasai operations
Kasai operations have a long tradition at the MHH. It is performed on newborns or very young infants with biliary atresia. Many of these children are transferred throughout Germany. For many children, it remains a bridging to transplant therapy. Due to the high level of pediatric cardiological expertise at our center, children with congenital heart defects are also transferred to our center in order to remain connected here for further care of this complex multi-organ treatment. The anesthetic management of these children is challenging and is examined over a period of 10 years.
Completed studies
Nickel K, Schütz K, Carlens J, Grewendorf S, Wetzke M, Keil O, Dennhardt N, Rigterink V, Köditz H, Sasse M, Happle C, Beck CE, Schwerk N. Ten-year experience of whole lung lavage in pediatric pulmonary alveolar proteinosis. Clin Padiatr. 2024 Feb;236(2):64-72. doi: 10.1055/a-2194-3467.
Former doctoral students
| Dr. Anna Auf der Springe Compatibility of 6% hydroxyethyl starch 130/0.42 and 4% gelatine with intravenous drugs commonly used in pediatric anesthesia | Dr. Stefanie Arndt Influence of age on monitoring the depth of anaesthesia with the EEG-based Narcotrend Index during sevoflurane anaesthesia in children under 2 years of age |
| Dr. Katja Brunsmann Validation of a structured team briefing to increase patient safety in pediatric anesthesia at a university hospital | Dr. Frederike Elfgen-Schiffner Influence of etomidate on systemic and regional cerebral perfusion in neonates and infants with congenital heart defects |
| Dr. Tara Gashemi An observational study of the feasibility of monitoring exhaled propofol in children undergoing surgery under total intravenous anesthesia | Dr. Jonas Jürgens In vitro compatibility of acetate-containing balanced electrolyte solutions with drugs relevant to pediatric anesthesiology |
| Dr. Simon Zumsande Concentration measurement of volatile anesthetics under simulated trigger-free pediatric anesthesia |