Anatomy
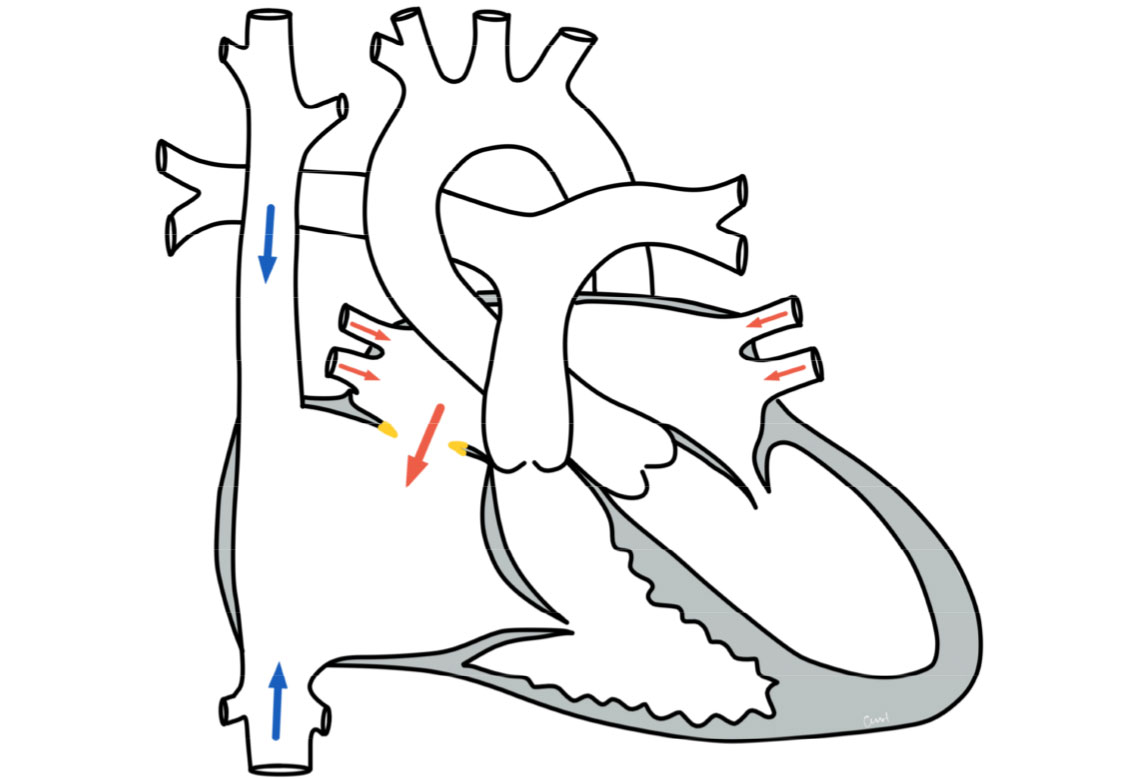
Anatomically, the two ventricles (atria) are separated from each other by a septum. In an ASD II, there is a connection between the left and right atrium through an interruption in this septum.
The defect is often located approximately in the middle of the atrial septum, in the area of the so-called foramen ovale (the opening between the two atria in the unborn child, which usually closes after birth). The size of the defects varies.
Physiology and hemodynamics
Depending on the size of the connection, more or less blood flows through the defect. As there is a slightly higher pressure in the left atrium, blood flows through the defect from the left into the right atrium (left-to-right shunt), from there into the right ventricle and then into the pulmonary vessels. This can lead to a strain on the right heart and to an over-perfusion of the lungs.
Unlike a ventricular septal defect, however, an atrial septal defect usually does not pose a risk of pulmonary hypertension, as the pressure in the two atria is significantly lower than in the main chambers. Therefore, although an atrial septal defect increases the blood flow to the lungs, there is no significant pressure load.
Therapy for a secondary type atrial septal defect
Conservative
The need for treatment depends on the size of the defect and therefore on the effects on the circulation (hemodynamic relevance). In many cases of small atrial septal defects, no special therapy is necessary; these can also close spontaneously over time. However, even the smaller atrial septal defects can cause problems over the years. For example, blood clots formed as part of a thrombosis can travel via the vena cava into the right atrium, via the defect to the left side of the heart and thus, for example, into the head vessels and cause a stroke. Drug therapy is not necessary in most cases.
Surgery and intervention
Depending on the location and size of the defect, the definitive treatment is surgery or intervention using catheter technology. In most cases, cardiac catheterization is a less stressful and successful method of closing the defect. In order to decide on the appropriate treatment procedure, planning is necessary with the help of preliminary echocardiographic examinations to visualize the size, location and shape of the defect. Most defects can be closed in the catheter laboratory. Using a cardiac catheter, a small umbrella is positioned in the defect through a vascular access (sheath) inserted into the inguinal vessels so that the defect is closed. It takes approx. 3-6 months for the umbrella to grow in completely. It is then completely covered by the inner lining of the heart, the endocardium.
If interventional closure is not possible (e.g. insufficient edge to hold an umbrella or too large a defect), surgical closure is performed. Surgical closure is performed using the heart-lung machine, with either an anterior approach through the chest or an oblique approach with a small incision (MIS technique). The defect is closed with a patch made of pericardial material or other tissue (synthetic or biomaterial). After the operation, the patient is treated briefly in the intensive care unit before returning to the cardiology follow-up ward.
Prognosis for a secondary type atrial septal defect
Further course
After closure of an atrial septal defect, children or adults are in good heart health. After interventional closures, annual check-ups are recommended. After timely therapeutic closure, normal physical resilience and an unimpaired lifestyle can be expected.
