The team for congenital heart defect surgery under the direction of Dr. Horke performs over 250 operations on the heart and great vessels every year - making Hannover Medical School one of the largest centers for congenital heart defects in Germany.
State-of-the-art technology and surgical procedures are just as much a matter of course as forward-looking planning for a whole and healthy life. The cardiosurgery team consists of several fully trained cardiosurgeons specializing in congenital heart defects. Surgery not only includes the correction of heart defects in infancy, but also covers the entire spectrum of operations on congenital heart defects - right through to old age. On these pages you will find information on our surgical procedures and innovative valve replacement materials - tissue-engineered heart valves for pulmonary and aortic valve replacement.
We have compiled information on the heart defects and the basic treatment options for you in a clear format in the heart defect overview.
More information on congenital heart defects More information on the tissue-engineered heart valve



The tissue-processed valve - "Hanover valve"
Occasionally, cardiac surgery for a congenital heart defect cannot completely correct the heart defect - for example, the anatomy of a pulmonary valve in patients with tetralogy of Fallot (TOF) sometimes prevents it from remaining functional for a lifetime. A replacement for this valve must then be carried out in the course of the patient's life. It would be desirable to have a valve that lasts a lifetime - but this type of valve replacement does not yet exist.
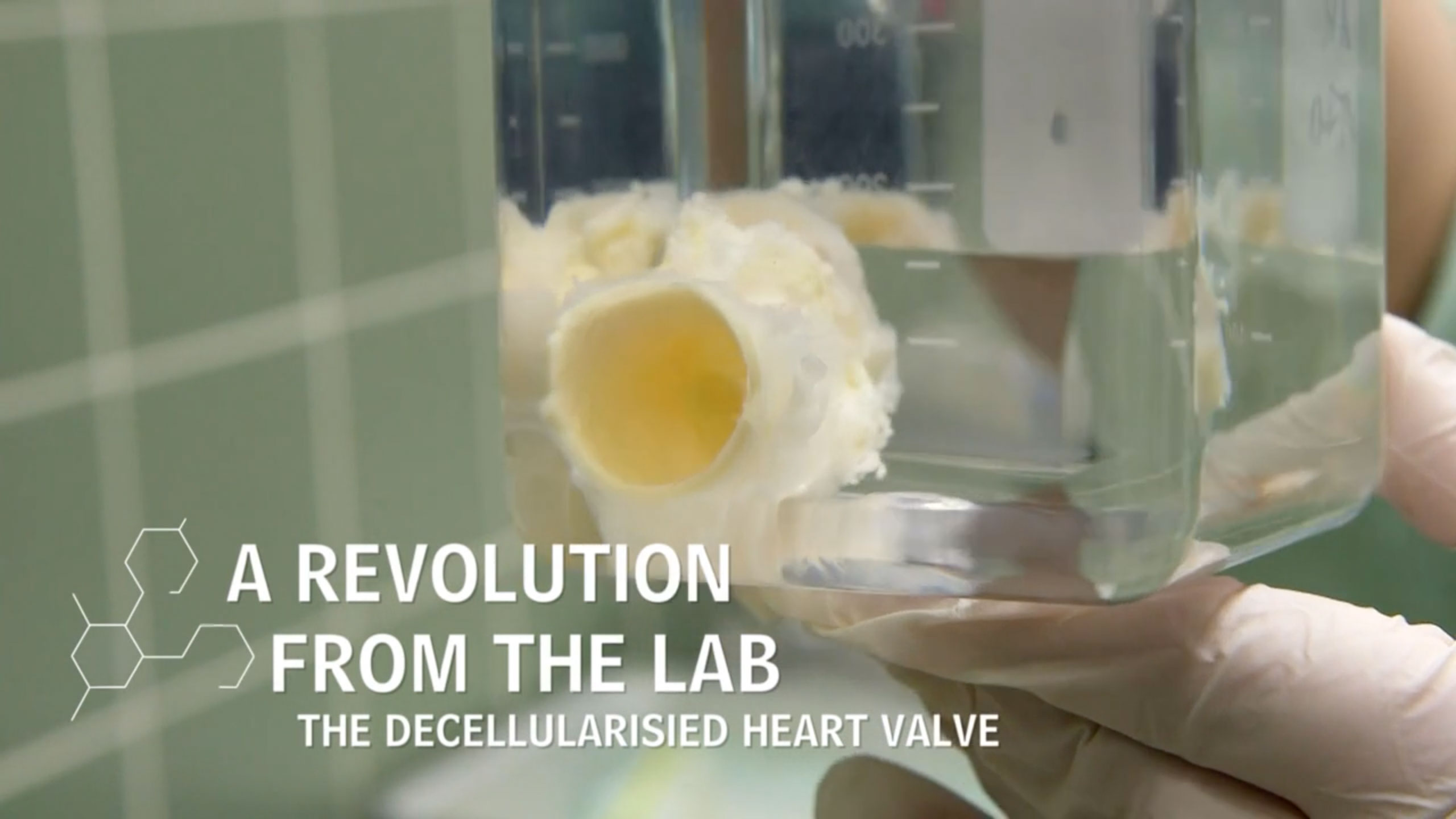
We are working on making the valves last as long as possible - a procedure has been developed at Hannover Medical School that completely removes the cells from donor valves. This leaves a scaffold that can then be repopulated by the body's own cells. The hope is that this type of treatment will create a valve that can adapt to the conditions in the body. Ideally, the size of the valve will also change with the size of the vessels ("growing heart valve").
More information on research on the "Hannover valve" in aortic position More information on research on the "Hannover valve" in Pulmonary Disposition
Cardiac surgery - like all areas of medicine - is constantly evolving. In Hanover, a procedure has been developed to treat heart valves in such a way that all foreign cells are removed (TE valve: "tissue-engineered" valve means "tissue-processed" valve). This leaves a scaffold on which the body's own cells can spread after implantation. Ideally, the valve adapts to the changed conditions - and lasts a particularly long time.