Cross-consortium use case: ABIDE_MI – Efficiently aligning biobanks and data integration centres
The use case ‘Aligning Biobanking and DIC Efficiently’ (ABIDE_MI) is a joint project involving most of the German university hospitals in the four consortia of the Medical Informatics Initiative (MII). The aim of the project, which was launched in May 2021, is to enable the MII's data integration centres (DICs) to link patient data from routine care with data on biological samples and make it available for research purposes. In particular, researchers should be able to submit feasibility queries via the MII's future German Research Data Portal for Health.
CAIMed is Lower Saxony's research centre for artificial intelligence and causal methods in medicine.
CAIMed focuses on linking research data, clinical data and patient care data, as well as the use of artificial intelligence and causal methods. This enables prevention, diagnosis, therapy and monitoring of therapeutic success to become more effective and efficient, and the individual needs of each person to be better identified and met.
CAIMed develops innovative methods for improved, personalised healthcare and contributes to the management of common diseases such as cancer, cardiovascular disease and infections. By linking Lower Saxony's excellent locations for methodological AI research, data-intensive medicine, medical informatics and basic medical research, a unique beacon for research into AI and personalised medicine is being created.
The centre is supported by scientists from the L3S Research Centre at Leibniz University Hannover, Hannover Medical School, the Helmholtz Centre for Infection Research Braunschweig / Centre for Individualised Infection Medicine (CiiM), Georg August University Göttingen / Campus Institute for Data Science (CIDAS) and Göttingen University Medical Centre.
Hannover Medical School
The MHH is one of the most productive medical universities in Germany. Its research focuses on transplantation and stem cell research, regenerative medicine, infection and immunity research, biomedical engineering and implant research. In the field of medical informatics, numerous projects related to AI and big data have been acquired. In addition, L3S and MHH are working closely together in the ZDIN's Future Lab Health. The MHH operates a clinical data warehouse with data from more than 2 million patients, a data integration centre for the Medical Informatics Initiative, and the largest biobank in Germany with over 1 million patient entries.
COVID-19 Research Network Lower Saxony (COFONI)
The COVID-19 Research Network Lower Saxony (COFONI) supports eleven research projects with the aim of better understanding SARS-CoV-2 infection and its consequences. The Lower Saxony Ministry of Science and Culture (MWK) is providing a total of €8.4 million in funding to establish the COVID-19 Research Network, which brings together the core scientific competencies of the Göttingen-Hanover-Braunschweig metropolitan region.
The research project of BioMaterialBank (BMB) Nord in Borstel, HUB in Hanover, PopGen in Kiel, ICB-L in Lübeck, IRB in Greifswald and IBBJ in Jena builds on a cooperative basic project of the Research Centre Borstel in the field of pulmonology. The motivation is to generate reference values for healthy individuals. As part of the proposed project, joint decentralised recruitment of healthy volunteers (n=250) is planned across five differently structured locations and recruitment strategies.
Sample collection, processing, management, storage and transport will also be carried out decentrally in BMBs with different infrastructures. The objectives of the research project are (A) to provide high-quality and, as far as possible, comparable BMPs, (B) the central analysis of decentralised BMPs using various analytical methods at one of the sites, the determination of reference values for scientific questions, (C) the identification of critical factors in decentralised recruitment, collection and processing of BMPs and the development of generic recommendations and standards, as well as the provision of results in internationally usable formats.
Hepatitis D is by far the most severe form of chronic viral hepatitis, often leading to liver failure, hepatocellular carcinoma and death. However, knowledge about the pathophysiology of the disease and the interactions between host and virus is very limited, which explains the large interindividual variability in the course of hepatitis D.
The D-SOLVE consortium (‘Understanding the individual host response to the hepatitis D virus to develop a personalised approach to the treatment of hepatitis D’) aims to conduct unbiased screening of a large multicentre cohort of well-defined HDV-infected patients in order to better understand the individual factors that determine the outcome of the infection and to identify individuals who will benefit from currently available treatments.
Three sub-projects are being established within the D-SOLVE consortium. The first takes a cross-sectional approach, covering 750 patients who reflect the entire spectrum of HDV infection in Europe. The second consists of a retrospective prospective cohort of patients with liver biopsies taken 10 to 20 years ago to enable the investigation of intrahepatic immune correlates with disease progression, and the third will be a prospective study of patients treated with the novel inhibitor bulevirtide.
General information about the DZL
Lung diseases are among the most common causes of death in Germany and worldwide and represent diseases with a high disease burden. Currently, there are few effective treatment options for most chronic lung diseases. In order to treat lung diseases more successfully in the long term, research must address these challenges in a scientifically and structurally coordinated manner.
DZL location in Hanover
Since 2011, Hanover has been funded by the Federal Ministry of Education and Research (BMBF) as one of five locations of the German Centre for Lung Research (DZL). At that time, Hannover Medical School (MHH) applied together with the Fraunhofer Institute for Toxicology and Experimental Medicine (ITEM) and Leibniz University Hannover as a joint network called BREATH (Biomedical Research in Endstage And ObsTructive Lung Disease Hannover) and impressed with its concept.
http://www.breath-hannover.de/
DZL – German Centre for Lung Research
The German Centre for Lung Research (DZL) is a consortium initiated by the BMBF (Federal Ministry of Education and Research) with the aim of jointly developing more effective therapies for lung diseases and new options for prevention and diagnosis. The focus is on basic research closely linked to clinical practice. In a bidirectional process, the results of basic research are to be quickly transferred to clinical medicine.
The DZL is an association of leading university and non-university institutions for lung research with the aim of comprehensively investigating the eight diseases or disease groups that are the focus of attention.
- Asthma and allergies
- Chronic obstructive pulmonary disease (COPD)
- Cystic fibrosis
- Acute lung injury and lung failure
- Interstitial lung diseases
- Pulmonary hypertension
- Severe end-stage lung diseases
- Lung cancer
Deutsches Zentrum für Lungenforschung (DZL)
Although antibiotics and vaccines have been used successfully for decades, infections continue to be responsible for an immense number of illnesses and deaths worldwide. In addition to chronic and poverty-related infectious diseases, major challenges include emerging microbial and viral infections, which spread rapidly across the globe via modern transport routes. The rapid emergence of resistance to anti-infective agents on the market poses another serious threat. Added to this are infections in immunosuppressed patients, who are being treated with modern high-performance medicine, particularly in the fields of transplantation and oncology.
Combating infectious agents and the associated health threats requires new, integrative and interdisciplinary approaches in which experts in the fields of translational basic research, epidemiology and clinical medicine work closely together. In 2011, the Federal Ministry of Education and Research founded the German Centre for Infection Research, which brings together universities, university hospitals, Leibniz and Max Planck Institutes, Helmholtz Centres and federal research institutions with a strong profile in the field of infectious diseases in order to address the most important infectious disease challenges with an integrative approach.
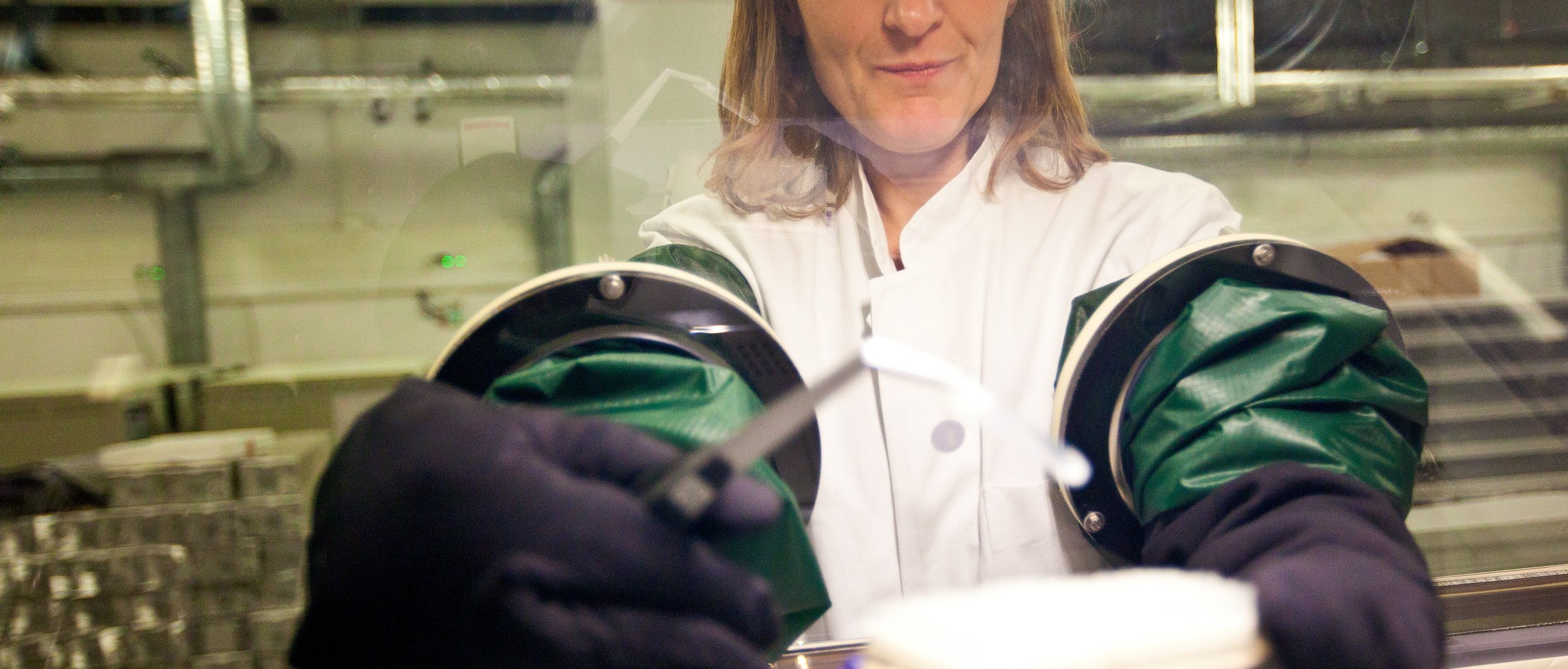
TI Biobanking
A comprehensive biobank structure is essential for conducting infection research at many different locations and for translating the results of this research into practical applications.
Biomaterials of great relevance to DZIF partners include cultures of pathogens and cultures of so-called microbial producers, i.e. bacteria that are suitable for the production of active substances, as well as liquid biological samples such as serum, plasma and urine, and well-characterised tissue samples from infected patients.
A coordination office and a technology platform have been set up within the DZIF's ‘Biobanks’ unit. The DZIF's Heidelberg site coordinates tissue biobanking. The German Collection of Microorganisms and Cell Cultures (DSMZ) provides standards and protocols for the storage, maintenance, authentication and quality control of strains of microbial pathogens and microbial producers. The Munich site is responsible for the biobanking of liquid samples.
The biobank platform is a resource and technology platform for the DZIF that
- provides high-quality biomaterials linked to clinical data
- supports biobank activities at partner sites with the help of roll-out programmes, and
- promotes the harmonisation/standardisation of workflows and ELSI, IT, QM and IP solutions within the DZIF.
The biobank platform is based on existing and future biobanks and collections within DZIF and their expertise and organisational structures.
It cooperates with national (TMF) and international (BBMRI, EMbaRC, GBRCN) players in the field of biobanking and draws on their generic concepts.
Objectives of the DZIF Biobank Platform
The DZIF Biobank Platform aims to provide DZIF projects and their partners with secure, high-quality, authenticated and standardised biomaterial and its derivatives.
Specifically, the following objectives are to be achieved:
- Establishment and coordination of a DZIF bioresource platform
- Establishment and characterisation of collections of microbial pathogens and drug producers as well as human biomaterial and corresponding derivatives (DNA, RNA, metadata, cell lines) for DZIF and other partners at the DZIF locations
- Establishment of a methods platform for obtaining derivatives and optimised analyses
- Establishment of a database, a ‘virtual bioresource centre’, in which the metadata available for the samples is made available to DZIF partners
- Creation of structured ELSI, QM and IT solutions for DZIF biobanks and partners
http://www.dzif.de/infrastruktur/biobanken/
The DZIF transplant cohort is part of the research area ‘Infections in immunocompromised hosts’ at the German Centre for Infection Research (DZIF) and is specifically geared towards the needs of patients who have received a donor organ or stem cell transplant.
Background
Recipients of donor organs are dependent on lifelong medication to prevent rejection of the new organ. These immunosuppressants weaken part of the body's immune response. This protects the new organ, but leads to increased susceptibility to infections. Organ recipients are therefore particularly at risk from pathogens. Recipients of stem cells also initially have a greatly reduced immune defence due to the underlying disease and treatment.
This means that infections occur more quickly than usual and can lead to complications. If an organ has been transplanted, infections can impair the function of the organ and, in the worst case, lead to failure of the new organ.
The individual risk of patients experiencing complications depends on many different factors. The better the relationships between the type of transplant, pre-existing conditions, medication and infections are understood, the better prevention and treatment can be carried out in practice.
Objectives
With the help of the transplant cohort, medical data and biological samples from transplant patients throughout Germany can be collected and managed. These data and samples form the basis for scientific studies. These studies examine the relationships between the numerous factors that can influence susceptibility to infection and organ function. In collaboration with the participating clinics and research institutions, we aim to promote the exchange of experiences and gain new knowledge. The study results may lead to new insights and continuous improvements in the treatment of transplant patients.
Collected data and samples
An essential component of the transplant cohort is the cohort database, which is operated by the Institute for Medical Statistics and Epidemiology at the Klinikum rechts der Isar hospital in Munich.
This database collects information that can provide insights into the individual infection risk of transplant patients. This includes information on pre-existing conditions, existing infections, the course of the transplant, medication and infectious events that occur. A specific set of parameters was defined in advance for each organ so that the events relevant to the type of transplant are taken into account.
Biomaterial from transplant patients serves as another important basis for later studies. Only samples that are collected during the routine treatment of patients and are no longer needed for further examinations are used. The biomaterials are stored in professional biobanks. To this end, the transplant cohort works closely with the DZIF Biobank Platform.
GAIN – German Network for Research and Therapy Optimisation for Patients with Multi-Organ Autoimmune Diseases
Autoimmune diseases that affect multiple organs are among the extremely rare diseases in humans. In these diseases, the body's own immune system mistakenly attacks its own organs due to a malfunction. Patients typically suffer from inflammation of several organs, such as the bone marrow, intestines, lungs, kidneys, skin and nervous system. Only recently have individual changes in genes that control the immune system been described as the cause of these clinical pictures.
The aim of the GAIN (German Auto-Immune Network) consortium is to improve understanding of the pathogenesis and treatment of patients with congenital immune system defects that lead to such autoimmune diseases. To this end, patient data will be collected and the identification, diagnosis and treatment of those affected will be standardised. Another goal is to analyse in greater depth both the development of individual diseases and the role of different cells and other controlling factors. In addition, the safety and efficacy of abatacept, a drug that inhibits certain components of the immune system, will be investigated in a subgroup of patients in a clinical trial.
The GAIN research network is part of the ‘translation-oriented joint projects in the field of rare diseases’. In the fourth funding phase for rare diseases, a total of eleven networks will be funded over three years. Expertise from across Germany will be brought together to develop new insights into rare diseases through problem-solving-oriented and interdisciplinary collaboration. Research into rare diseases also promises to yield model insights that can be transferred to other, more common diseases.
Biobanking HUB und Teilprojekt 10: Identifizierung epigenetischer Faktoren
Projektleitung: Dr. Faranaz Atschekzei
Im Netzwerk die Forschung stärken
Das German Biobank Network (GBN) vereint akademische Biobanken in Deutschland, die humane Bioproben sammeln und für die Forschung bereitstellen, und bietet ihnen eine gemeinsame Plattform zur Zusammenarbeit und Weiterentwicklung. Das GBN vertritt deutsche Interessen im europäischen Biobankennetzwerk BBMRI-ERIC und unterstützt die biomedizinische Forschung auf dem Weg zur Präzisionsmedizin.
Das heutige Netzwerk ist aus zwei eng verbundenen Strukturen hervorgegangen: dem German Biobank Node (GBN) als koordinierender Dachorganisation und nationalem „Knoten“ des BBMRI-ERIC sowie der German Biobank Alliance (GBA), die die kooperierenden Biobanken umfasste. Unter der Leitung des damaligen GBN schlossen sich 2017 Biobanken aus elf deutschen Universitätsklinika sowie zwei IT-Entwicklungszentren in der GBA zusammen. Seit 2025 sind Biobanken an 37 Standorten sowie ein IT-Entwicklungszentrum im Netzwerk aktiv. Die Biobank-Partner arbeiten nach einheitlichen Qualitätsstandards und machen Bioproben sowie die dazugehörenden Daten über eine vernetzte IT-Infrastruktur europaweit für die biomedizinische Forschung verfügbar.
Zum 1. Juli 2025 wurden beide Strukturen – GBN und GBA – unter dem neuen Namen German Biobank Network (GBN) zusammengeführt. Gleichzeitig wurde das GBN organisatorisch im Netzwerk Universitätsmedizin (NUM) verankert. Die neue Bezeichnung bringt die gewachsene Struktur und ihre Rolle als zentrale Infrastruktur für das Biobanking in der Universitätsmedizin zum Ausdruck.
Das NUM befindet sich seit dem 1. Juli 2025 in seiner dritten Förderperiode mit einer fünfjährigen Laufzeit, gefördert durch das Bundesministerium Forschung, Technik und Raumfahrt (BMFTR). Um die im NUM entstandenen Strukturen dauerhaft zu sichern, hat das BMFTR eine Verstetigung des Netzwerks über die aktuelle Förderperiode hinaus in Aussicht gestellt.
The future of hearing
The goal of the ‘Hearing4all’ cluster of excellence is literally ‘hearing for all’. By improving individualised hearing diagnostics and the provision of personalised hearing aids tailored to each individual, the scientists aim to significantly improve the communication situation for those affected – whether at work, in traffic or at home. To this end, fundamental model-based work is being carried out on the diagnosis and auditory profile of people with normal to severe hearing loss in order to gain a better understanding of individual hearing. In addition, these models are used to improve the individual provision of technical hearing aids and to optimise them for the respective situation.
Immune Safety Avatar: non-clinical simulation of the effects of immunomodulatory therapies on the immune system
The vision of Immune Safety Avatar (imSAVAR) is to develop a platform for integrated non-clinical assessments of the safety and efficacy of immunomodulatory therapies. Existing non-clinical models do not adequately represent the complexity of the immune system and its interactions in both immuno-oncology and immune-mediated diseases. Nor do they accurately reflect the diversity of responses to new therapies observed in clinical medicine.
We will therefore continuously refine and develop existing non-clinical models with the aim of validating (i) the value of non-clinical models for predicting the efficacy and safety of immunomodulators, including high-throughput cellular assays, complex organism models and microphysiological models (ii) developing new endpoints and better monitoring approaches for immune function testing, and (iii) developing cellular and molecular biomarkers for the early detection of side effects. The imSAVAR platform is based on case studies of prioritised therapeutic modalities and draws on Fraunhofer Society institutes with many years of experience in applied science, particularly in toxicology.
The consortium will work with the private sector, pharmaceutical companies, regulatory authorities and technology providers to improve the prediction of the transferability of the safety and efficacy of immunomodulators from preclinical models to human studies. We will share experience with customised models that can be used (in accordance with the 3Rs principles), set up the necessary infrastructure, perform the analyses and provide broader expertise on disease areas. This joint effort will ensure that the imSAVAR platform continuously benefits the field of immune safety assessment and creates opportunities for European companies. A guiding principle of this consortium is the meaningful engagement of multiple stakeholders, including patients and regulatory authorities. A multi-stakeholder community will be established.
Nationwide antibody study on the spread of SARS-CoV-2 infections
Multilocal and serial prevalence study on antibodies against SARS-2 coronavirus in Germany
The actual seroprevalence of SARS-CoV-2 in the population is crucial for better understanding the possible underreporting of infected individuals and for deriving decisions on the possible continuation or termination of interventions, as well as for enabling the precise determination of mortality rates and severe disease progression.
COVID antibody cohort:
Analysis of SARS-CoV-2 antibodies in the general population
- 60,000 subjects
- Healthy adults
- EDTA plasma
NEOCYST is a multidisciplinary, multicentre network for research into cystic kidney diseases in children. It is an association of clinicians, geneticists and scientists who share the common goal of improving the care, treatment and quality of life of patients with cystic kidney diseases.
Hereditary cystic kidney diseases are one of the most common causes of chronic kidney failure in children. At the same time, they belong to the group of ‘rare diseases’, meaning that only a few hundred patients in the UK are affected. All cystic kidney diseases are characterised by a high degree of phenotypic and genetic variability. In addition, significant disease overlap makes early diagnosis and individual counselling of affected patients and their families difficult.
NEOCYST aims to improve knowledge about the epidemiology, symptoms, genetics, molecular pathophysiology and long-term prognosis of cystic kidney diseases and associated syndromes in order to achieve targeted diagnostics, sound counselling and the development of future therapeutic approaches.
The project is funded by the Federal Ministry of Education and Research (BMBF) and supported by the Society for Paediatric Nephrology (GPN).
The parallel establishment of a biobank as a platform for disease-specific translational research helps to identify common ‘pathways’ in cyst formation and disease progression, with a particular focus on the control of cilia length, signal transduction and polarity of planar cells through the use of human biomaterials.
The focus of the biomaterial biobank subproject is on establishing a biomaterial collection from patients at the onset of cystic kidney disease.
The collection includes body fluids such as EDTA blood for plasma, DNA, serum, urine and primary cells. Within 3 years, approximately 200 patients will be involved in this project, with 60 patients recruited annually in up to 6 clinical centres of the NEOCYST consortium and their collaborating centres. The patients come for follow-up examinations
Harmonised SOPs ensure that sample generation, processing, storage and shipping are adapted to the standards of the German Centre for Lung Research (DZL), the TMF and the ISBER. The samples will be aliquoted into 2D barcoded cryotubes and frozen at clinical centres. Test registration will be carried out using a web-based registration tool.
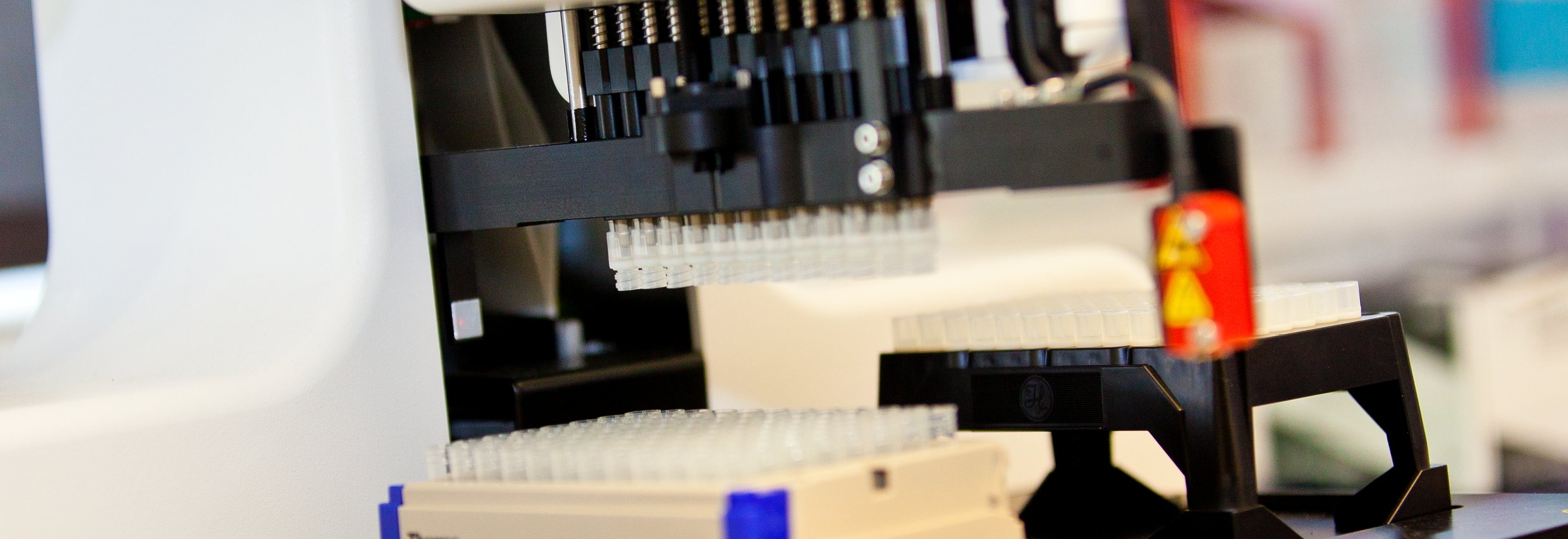
The frozen biomaterials from the clinical sites will be sent to the MHH Hannover Unified Biobank (HUB). At the HUB, the samples are registered, checked and stored in an automated warehouse at -80 °C. Two-thirds of the samples are stored for long-term storage in the gas phase of liquid nitrogen tanks. The remaining third of the samples remain in the automated warehouse to enable quick sample access for the consortium's sub-projects.
All processes are supported by modern, secure IT systems and meet the requirements of the TMF data security concept. A central study registry contains the patient-related phenotype data.
Further information:
National Research Network of University Medicine on COVID-19 (NUM) – National Pandemic Cohort Network (NAPKON)
National Pandemic Cohort Network:
The aim is to establish a harmonised, expandable and interoperable National Pandemic Cohort Network (NAPKON) in order to support the fight against the COVID-19 pandemic and its consequences, as well as future pandemics of any origin. The focus is on establishing a uniform concept with infrastructure cores and three cohort platforms for the representative collection of fine-grained data and biosamples.
Prof. Dr. Thomas Illig is head of the NUM Biosample HUB.
Building on the successes of NAPKON in 2020 and 2021, national collaboration across the three NAPKON cohorts will continue in order to fulfil the task of establishing a national collaborative infrastructure and making relevant contributions to the understanding and long-term management of the current SARS-CoV-2 pandemic (see NAPKON). NAPKON and NUKLEUS will further expand their close cooperation and leverage synergies with the NUM projects COVerCHILD, COVIM and the NAPKON Therapeutic Intervention Platform (NAPKON-TIP). The specific objectives of NAPKON v2 are to consolidate the infrastructure and generate new insights into COVID-19 and PCS (post-COVID-19 syndrome). The data and biosamples collected in the NAPKON cohorts will also be used for centrally conducted multi-OMICs analyses to investigate the pathophysiological mechanisms of COVID-19 and signatures that predict and cause specific outcomes and phenotypes of COVID-19 and post-COVID-19 syndrome (PCS). To this end, the project has been linked to the Sample Analysis for Post Covid Research in NAPKON (SAPCRiN) project.
SAPCRiN project on Long Covid
Every coronavirus infection carries the risk of long-term health damage. However, there is a lack of precise diagnostic criteria, scientifically sound findings on the pathophysiology and risk factors, and treatment options for Long Covid. With the aim of finding prognostic markers and treatment options for the disease, the SAPCRiN (Sample Analysis for Post Covid Research in NAPKON) project will start in early 2022 as part of a call for proposals from the Federal Ministry of Education and Research (BMBF) on Long Covid. The project is funded by the Network University Medicine (NUM). SAPCRiN will receive a total of around one million euros in funding over a period of two years.
National Pandemic Cohort Network (NAPKON) as a basis
SAPCRiN is based on NAPKON, the National Pandemic Cohort Network. NAPKON is an existing NUM project and provides an ideal platform for research into Long Covid. Within three different COVID-19 patient cohorts, clinical data, biosamples and imaging data from acutely ill or recovered COVID-19 patients are collected nationwide according to uniform standards. This allows the course of COVID-19 to be recorded and the relationship with comorbidities and other health parameters as well as the long-term effects to be investigated. To date, NAPKON has recruited more than 3,500 patients and followed them longitudinally. During each visit, standardised biological samples are collected at all participating university hospitals, which form the basis for the planned systematic molecular characterisation.
Signal effect for biobanking
"The fact that the SAPCRiN project can benefit from NAPKON is a significant advantage for Long Covid research. SAPCRiN encompasses RNA and DNA isolations as well as molecular analyses of one of the defining diseases of our time,‘ says project coordinator Prof. Dr. Thomas Illig, one of the five principal investigators of NAPKON, head of the German Biobank Alliance (GBA) partner site in Hanover and deputy spokesperson for the GBA. ’This is also a great success for biobanking in Germany."
Molecular changes and regulatory genes
Among the seven institutions involved is the Helmholtz Zentrum München with the Joint Biobank Munich (JBM), also a partner biobank of the GBA. Dr Gabriele Anton, deputy coordinator of the JBM, explains: "In the SAPCRiN project, we are characterising the molecular changes that occur during Covid-19 infection and the healing process, and investigating whether these changes are related to the development of Long Covid. Using longitudinal multi-OMICS data and health data from NAPKON patients, we are also identifying regulatory genes and associated molecular pathways that play a role in Long Covid."
In order to meet the challenges of current and future pandemics and address pressing medical research questions, a network is needed that can quickly focus the capabilities of university medicine on particularly urgent and important tasks and conduct complex clinical studies itself.
To this end, a therapeutic intervention platform (NAPKON-TIP) is to be established based on the recruitment network successfully established in the National Pandemic Cohort Network (NAPKON) and the NUM infrastructures, in particular the NUM Clinical Epidemiology and Study Platform (NUKLEUS).
NAPKON-TIP was designed as a platform for adaptive clinical studies, facilitating the ongoing evaluation of new therapies in terms of their efficacy and safety in stratified population groups.
NAPKON-TIP focuses on adaptive trials, which are unique in that the therapies and subgroups included can be adjusted if new findings on the efficacy and safety of the treatments and the stratification of the population within or outside the platform trial suggest this.
The NUM Clinical Epidemiology and Study Platform (NUKLEUS) provides infrastructure and specific expertise for the planning, implementation and evaluation of multicentre clinical and epidemiological studies. It offers the scientific community optimal access to infrastructure for the provision of high-quality data and biosamples.
The Biosample Core Unit (BCU) is responsible for the quality of biosamples and biosample-associated data in NAPKON and future NUM studies. High-quality biobanking, in particular the use of common standard operating procedures (SOPs) for the collection and processing of biosamples, is an important prerequisite for multicentre studies and ensures successful and reproducible research based on the collected biosamples. The BCU is headed by Prof. Dr. Illig from the Hannover Unified Biobank (HUB) and Dr. Anton from the HMGU in Munich.
Furthermore, the BCU has developed and implemented an audit programme that supports the various university hospitals in implementing uniform quality standards for the provision of high-quality data and biosamples.
NUKLEUS | Netzwerk Universitätsmedizin
Forschungsinfrastrukturen im NUM | Netzwerk Universitätsmedizin
Refugees are particularly susceptible to infectious diseases due to the living conditions caused by displacement and mass accommodation. Due to the generally low vaccination rates and the comparatively high prevalence of certain infectious diseases (e.g. COVID-19, HIV, HBV, HCV, TB, measles, chickenpox) in the Ukrainian population, expertise in infectious diseases is particularly in demand here. Specifically, a total of 2,500 refugees in the participating NUM centres will undergo a structured screening and vaccination programme in close cooperation with the health authorities. This also includes children, who are particularly affected and at risk of infection in the current wave of refugees. The data collected in this context will be systematically evaluated by NUM scientists in order to better identify the care needs of the group of war refugees and to be able to formulate appropriate recommendations.
With the NUM Study Network (NUM SN), we aim to develop an effective system of cooperation in the field of clinical and clinical-epidemiological studies in Germany. We work closely with existing infrastructures, networks and researchers and seek to support this process through organisational and structural measures. Study managers should be relieved of administrative and operational tasks by consistently simplifying these tasks and transferring them to study support structures. This will enable more studies to be initiated in less time, more patients to be recruited for studies within a reliable timeframe, and the quality of data and biosample collection to be improved.
The NUM SN builds on the preliminary work of the National Pandemic Cohort Network (NAPKON), the NUM Clinical Epidemiology and Study Platform (NUKLEUS) and the NUM Data Integration Centres (NUM-DIZ). These established concepts and the resulting infrastructures, organisational units and experience serve as the basis for a gradually growing, high-performance network for the efficient conduct of clinical and clinical-epidemiological studies in Germany and are being rolled out uniformly among the participating network partners.
Personalised medicine to combat depression
MHH Psychiatry coordinates largest German study to improve depression treatment
RESIST Cluster of Excellence for Infection Research
The RESIST Cluster of Excellence aims to improve our understanding of individual susceptibility to infections so that we can prevent, diagnose and treat infections in a tailored manner. ‘This is a great day for infection research and thus for people who are particularly susceptible to infections – whether due to congenital immune deficiencies, a suboptimally developed immune system or as a result of medical therapies. Infections can be particularly harmful to them, and we look forward to improving the possibilities for diagnosis and therapy in the long term,’ said Professor Dr Thomas Schulz. The head of the MHH Institute of Virology is the spokesperson for this regional network, which includes the Helmholtz Centre for Infection Research, the TWINCORE Centre for Experimental and Clinical Infection Research, the Veterinary University Foundation, the Centre for Structural Systems Biology (CSSB) in Hamburg and the Centre for Chronic Immunodeficiencies (CCI) in Freiburg.
Newborns and the elderly, whose immune systems are not yet developed or are very vulnerable, as well as people whose immune systems are suppressed for therapeutic reasons, such as in multiple sclerosis or after a transplant, are particularly susceptible to infections. But infections can also be dangerous for people with implants.
In order to combat infections more effectively than before, the RESIST team will investigate the molecular basis of immune deficiencies against pathogens and develop diagnostic procedures that will allow better assessment of individual susceptibility to infection, enabling more personalised treatment.
RESIST conducts basic research and aims to identify new approaches that can be developed in existing translational programmes, for example in the German Centres for Infection and Lung Research, the Clinical Research Centre and the Centre for Individualised Infection Medicine. In the long term, the new findings obtained in RESIST will be incorporated into these centres and further developed for application in patients.
Research of DZL / BREATH
ABACOPD study – Randomised, double-blind, placebo-controlled study to prove that antibiotics are not necessary for moderate acute exacerbations of COPD.
What is asthma – and if so, how many? Based loosely on a popular book title, one could also define the question posed by the All Age Asthma Cohort (ALLIANCE). In fact, doctors recognise not just one type of asthma, but a variety of typical disease progression patterns. A good quarter of all children experience wheezing at least once in early childhood. This is a typical sound when exhaling, caused by narrowed airways. Although it can be a sign of later asthma, only 3-5% of all children who wheeze or show other early symptoms retain their asthma into adulthood. In other cases, asthma only occurs in adulthood, but then often in a severe form.
In order to predict how a disease will progress and how it should be treated, the German Centre for Lung Research (DZL) established the ALLIANCE cohort during its first funding period. It now includes more than 1,000 patients and healthy subjects between the ages of six months and 84 years. After a comprehensive baseline examination, asthma patients usually visit the respective study centres once a year. Healthy subjects, who serve as a control group, are examined once.
As part of the examination programme, the ALLIANCE study team measures the subjects' lung function and airway inflammation and tests the extent to which they are sensitised to certain allergens. Biomaterials such as blood, nasal swabs, sputum and exhaled air are collected and analysed. Structured questionnaire interviews and data from patient records document symptoms, disease progression, living conditions and environmental factors. In order to be able to directly compare the results in children and adults, the range of examinations is designed to be as similar as possible and the procedures are standardised.
A whole range of in-depth molecular biological analysis methods (“deep phenotyping”) will be used to elucidate the mechanisms of the various courses of the disease. The ALLIANCE cohort's data and biobanks now comprise hundreds of thousands of data points and patient samples. Their analysis has already begun. The aim of the study is to identify biomarkers (signal transmitters) that will enable the respective subtype of the disease to be detected as early as possible in the future. This would also make it possible to tailor treatment much more individually to each patient.
ALLIANCE is one of the DZL's major flagship clinical projects. The sites involved are ARCN (Kiel/Lübeck/Borstel/Großhansdorf), BREATH (Hanover), CPC-M (Munich) and UGMLC (Giessen/Marburg/Bad Nauheim), as well as the University Hospital of Cologne as a non-DZL partner. The paediatric part of the project involves collaboration between the University Medical Centre Schleswig-Holstein (Lübeck campus), Hannover Medical School, Giessen-Marburg University Hospital, Munich University Hospital and Cologne University Hospital. Adult patients are participating in the study at the LungenClinic Grosshansdorf and the Research Centre Borstel.
Sepsis is a life-threatening host response to infection with consecutive organ failure.
The lungs are very often affected in the form of ARDS (adult respiratory distress syndrome).
The ARDS Register and Biobank is a single-centre, prospective registry study with preservation of biomaterial (plasma/serum/DNA/urine/BAL).
Competence Network for Community-Acquired Pneumonia
Community-acquired pneumonia (CAP) is considered one of the most significant infectious diseases worldwide. It is associated with a high risk of mortality. In Germany alone, around 680,000 people contract CAP every year, a significant proportion of whom require hospital treatment. Despite the medical and health economic significance of this disease, there was a lack of reliable data in Germany on the spectrum of pathogens, the resistance situation of the pathogens and the course of the disease. For this reason, the BMBF initiated the Competence Network ‘Community-Acquired Pneumonia’ (CAPNETZ) in 2001. The aim of CAPNETZ is to reduce the number of people who contract pneumonia and die from it. To achieve this, diagnostics, therapy and patient care must be improved.
CAPNETZ brings together general practitioners and clinicians as well as microbiologists, virologists, epidemiologists and computer scientists. Leading research institutions in Germany cooperate in CAPNETZ. All clinical and microbiological data is collated and managed in a central material and database. By 2013, more than 10,000 patients had already been recorded in this way. About one-third of these patients were receiving outpatient treatment, and about two-thirds were admitted to hospital. The responsible pathogens are cultured and their sensitivity to antibiotics is determined. All clinical and microbiological data are collated and managed in a central material and database. CAPNETZ thus has the world's most comprehensive database on community-acquired pneumonia.
Available samples:
- Serum
- Plasma
- PBMCs
- Throat washings
- Urine
- Bacterial isolates
- Respiratory material
- EDTA blood
Patients:
Approximately 129,000 biological samples from approximately 14,236 CAP patients (2025)
(400 patients/year)
Further information:
Der Verbund COSYCONET im Kompetenznetz Asthma und COPD
The COSYCONET consortium in the Competence Network for Asthma and COPD
Chronic obstructive pulmonary disease (COPD) continues to pose a major challenge for medical practice. This is because the morphological and functional changes associated with COPD often affect not only the lungs, but also involve clinically relevant comorbidities. The connection between these comorbidities and COPD and the resulting interactions may be mediated by systemic inflammation.
This is the starting point for the COSYCONET consortium, which comprises a total of seven subprojects (SP). COSYCONET stands for German COPD and Systemic Consequences – Comorbidities Network.
The aim of subproject 1 is to establish a national COPD cohort with the support of specialist pulmonology clinics, university departments and practising pulmonologists, which can serve as a basis for long-term follow-up and a wide range of specialised studies. This large-scale, multicentre cohort study includes approximately 2,800 patients with all degrees of COPD severity. It has the status of a ‘national COPD cohort’. The patients were initially examined during an initial visit using a wide range of instruments. Further examinations will take place 6, 18, 36 and 54 months later. The individual examinations have already been used successfully in other studies or are part of new recommendations for the characterisation of patients with cardiopulmonary diseases.
In addition to lung function, the examinations aim to record as comprehensively as possible the individual pattern of comorbidities such as cardiovascular disease, osteoporosis, metabolic and mental status, physical performance and activity. In addition, blood samples are collected and stored and analysed in a biobank (TP4) to determine markers of systemic inflammation and ageing as well as organ-specific markers. Furthermore, CT images are evaluated using semi-quantitative analysis (TP5), provided they are available independently of the study.
The data collected will be compared with that of two population-based control cohorts, KORA (TP2) and SHIP (TP3). Health economic analyses (TP6) will round off the investigations.
Was the cancer treatment successful? How likely is it that the tumour will return? These are questions that concern both patients and doctors during follow-up care after treatment. The answers to these questions determine how often a patient must come to the hospital for check-ups, which can sometimes be stressful. To improve this process, the DZL recently launched the EMoLung study.
All five DZL sites are recruiting patients with early-stage disease for the EMoLung study*. The clinical research teams continuously collect blood samples and condensates of the study participants' exhaled air. The first sample is taken shortly before surgery, with all subsequent samples taken over the following two years. The scientists search for tumour DNA in the blood, while examining the respiratory condensates for specific ribonucleic acids (RNAs). The aim is to build on preliminary work from the first DZL funding period to find a so-called tumour signature that distinguishes patients with early recurrence from those who experience it late or not at all. The focus is not on genetic mutations, but on epigenetic changes* triggered by influences such as diet, lifestyle and exposure to pollutants (e.g. smoking). The result is a dysregulation of a number of genes. We want to use EMoLung to find out which genes these are.
Prof. Martin Reck from the LungenClinic Grosshansdorf is leading the study together with Prof. Ole Ammerpohl (University Hospital Ulm/University Hospital Schleswig-Holstein, Kiel Campus) and PD Dr. Guillermo Barreto (Max Planck Institute for Heart and Lung Research, Bad Nauheim). Ammerpohl and Barreto are conducting the epigenetic analyses in their laboratories. In addition to Großhansdorf, patients from the Hannover Medical School, the University Hospitals of Giessen and Heidelberg, the University Hospital of Munich and the Asklepios Specialist Clinics in Gauting are also participating.
The standard of follow-up care is currently computed tomography (CT), which is costly and stressful for patients. ‘If breath and blood analysis could complement CT and enable faster diagnosis of recurrence, this would be a major advance,’ says study leader Martin Reck. Blood sampling, a “liquid biopsy”, can be performed quickly and without significant risk. To obtain the breath condensate, the patient only needs to breathe into a tube for ten minutes. If successful, it should be possible to make the course of the disease more predictable and to better tailor monitoring and possible therapies to it.
Detecting lung cancer at an early stage: this is the goal of the HANSE study, funded by the German Centre for Lung Research (DZL) and the Lung Ambition Alliance, Germany's largest early detection programme. Since July 2021, the Hannover Medical School (MHH), one of three study locations in northern Germany, has been inviting (former) smokers between the ages of 55 and 79 to have their lungs checked. The prerequisite: an increased risk profile for lung cancer. Since then, over 600 participants have undergone lung cancer screening at the Hanover site. One of them is 72-year-old Gerhard Lunow. For him, the diagnosis came in time: the cancer was detected at an early stage and treated successfully.
For patients with severe end-stage lung diseases, such as COPD, the only curative treatment option currently available is lung transplantation, which is, however, reserved for a highly selected group of patients. In lung transplantation in particular, there is a growing mismatch between potential organ recipients and organ donors, leading to a progressive mortality rate among patients on the waiting list.
pedCAPNETZ: Reducing morbidity and mortality in children and adolescents with CAP through improved management
Lower respiratory tract infections are widespread among children and are associated with high morbidity and mortality, especially in the first years of life. One of the main pathogens is respiratory syncytial virus (RSV). Other relevant pathogens include human metapneumovirus, rhinovirus, influenza virus and the novel coronavirus SARS Cov2. To date, there is no specific treatment for respiratory infections caused by RSV and co-circulating viral pathogens in children and infants. The monoclonal antibody palivizumab is available for the prophylaxis of severe RSV disease in at-risk children.
The systematic collection of pathogen spectra, disease progression and treatment courses in paediatric clinics and paediatric practices should contribute to establishing measures for the treatment and prevention of severe respiratory infections and secondary diseases such as pneumonia. The socio-economic burdens associated with the diseases are also being collected as part of the PAPI study.
Porto-pulmonary hypertension is precapillary pulmonary hypertension associated with liver disease or portal hypertension.
NeoNeoAdjuvant Dynamic marker - Adjusted Personalized Therapy comparing sacituzumab govitecan versus sacituzumab govitecan+pembrolizumab in low-risk, triplenegative early breast cancer
1. Patient population:
- Any gender
- Pre- or post-menopausal
- With invasive, untreated triple-negative breast cancer
- Low to moderate clinical risk of recurrence (stage I and II)
2. Study design:
- Multicentre
- Interventional, phase II
- Two-arm Randomised
- Prospective
- Open-label, controlled
3. Study objectives:
The aim of the ADAPT-TN-III study is to investigate a well-tolerated and highly effective de-escalated therapy for early triple-negative breast cancer with the aim of avoiding longer and more toxic treatments. The study will investigate whether the combination therapy of sacituzumab govitecan + pembrolizumab achieves a higher rate of pathological complete remission than therapy with sacituzumab govitecan alone. Furthermore, 3-year survival in both arms will be investigated in comparison with historical controls.

ADAPTcycle - Mammakarzinome
Adjuvant dynamic marker – Tailored personalised therapy comparing endocrine therapy plus ribociclib versus chemotherapy in intermediate-risk, HR+/HER2- early-stage breast cancer

Neoadjuvant, dynamic marker-adjusted, personalised treatment of early HER2-positive breast cancer with trastuzumab deruxtecan compared to paclitaxel/docetaxel + carboplatin + trastuzumab + pertuzumab
1. Patient population:
- Female patients
- Pre- or postmenopausal
- With invasive, untreated HER2+ breast cancer Diagnosed no more than 6 weeks prior to registration
- Low, medium or high clinical risk of recurrence
2. Study design:
- Multicentre
- Interventional, phase II
- Two-arm Randomised
- Prospective
- Open-label, controlled
3. Study objectives:
ADAPT-HER2-IV is planned as a superiority study to demonstrate higher pCR (pathological complete remission) rates in both clinically relevant subgroups of HER2+ early breast cancer with low to moderate risk. In addition, it aims to investigate excellent survival in patients treated with T-DXd and thus demonstrate whether optimisation/de-escalation of therapy for early HER2+ breast cancer is possible with this approach.
Studien - Westdeutsche StudiengruppeWestdeutsche Studiengruppe (wsg-online.com)

New treatment option for patients with early breast cancer and increased risk of recurrence – study with abemaciclib
A randomised, controlled, open-label, phase III trial on adjuvant dynamic marker-adjusted personalised therapy comparing abemaciclib combined with standard adjuvant endocrine therapy versus standard adjuvant endocrine therapy in (clinical or genomic) high-risk, HR+/HER2- early breast cancer
German title:
A randomised, controlled, open-label, phase III adjuvant, dynamic marker-adjusted, personalised therapy study comparing abemaciclib plus standard endocrine therapy versus standard adjuvant endocrine therapy alone in hormone receptor-positive, HER2 receptor-negative early-stage breast cancer with a clinically or genomically high risk of late recurrence.
The study (ADAPTlate) is investigating whether the risk of local recurrence or metastasis in patients with hormone-dependent breast cancer can be reduced with the help of extended anti-hormonal therapy.
1. Patient population:
- Patients with early-stage breast cancer (non-metastatic)
- HR-positive
- HER2-negative
- Primary diagnosis no more than 6 years ago
- Inclusion in the study possible from primary diagnosis, randomisation only after completion of local treatment of breast cancer
- Planned or ongoing endocrine therapy
- Known high clinical or high genomic risk or intermediate clinical risk with unknown genomic risk
2. Study design:
This is a multicentre, interventional, prospective, two-arm, randomised, open-label, controlled, adjuvant phase III study to investigate the efficacy and safety of treatment with abemaciclib combined with endocrine therapy (ET) compared to standard endocrine therapy in patients with early-stage breast cancer (EBC) with the molecular subtype HR+/HER2-
3. Study objectives:
The objective of this ADAPTlate Phase III study is to determine whether the ‘late’ use of abemaciclib in adjuvant therapy is able to improve the outcome in early breast cancer for patients at high risk of recurrence.

Over the past 18 years, newly emerging coronaviruses have caused two epidemics and, most recently, a severe pandemic that has claimed thousands of lives. The extent of the current pandemic is not yet clear. Rapid action is needed to mitigate the consequences of the current pandemic and, beyond that, to better prepare us for newly emerging coronaviruses in the long term.
A consortium of scientists and physicians from the MHH and the Helmholtz Centre for Infection Research is participating in the establishment of a cohort of COVID-19 patients, and intensive molecular characterisation of this cohort is also planned. The cohort will enable a better understanding of the pathophysiology of the disease and the detection of biomarkers for severity and associated metabolic pathways, as well as treatment options for the disease.
The COVID-19 cohort will comprise a total of 1,000 patients with varying degrees of disease severity and control subjects. Samples of blood, living blood cells, plasma, serum, saliva, and bronchoalveolar lavage (BAL) will be collected and stored in the biobank (Hannover Unified Biobank/HUB). Sample collection and processing has already begun at the Hannover Unified Biobank (HUB), the central biobank of the MHH.
Funding for the project has been approved by the MWK (Lower Saxony Ministry of Science and Culture). Further funding for COVID-19 projects is being sought in close cooperation with the German Centre for Infection Research (DZIF) and the DZIF-Tx cohort, among others.
Biomaterials:
Blood, PBMCs, plasma, serum, buffy coat, saliva, and bronchoalveolar lavage (BAL)
Patient numbers:
A total of 1,000 patients with varying degrees of disease severity and control subjects are planned.
The national DIGIT-HF study is entering its second funding period.
In Germany, around three million people suffer from chronic advanced heart failure. The disease is one of the most common reasons why patients have to be admitted to hospital or die from the consequences. In this large multicentre study, scientists from the Department of Cardiology and Angiology at Hannover Medical School (MHH) are testing the efficacy of the drug digitoxin. More than 800 patients in around 40 centres have already been enrolled in the DIGIT-HF study.
Further information:
Fanconi anaemia (FA) is a rare, inherited disorder characterised by progressive bone marrow failure, various congenital anomalies and a predisposition to malignancy. There is phenotypic heterogeneity among patients with FA, which can be attributed to at least 16 gene mutations. The FA Registry was established to better define and understand the natural course of the disease and its genetic and environmental modifiers. The registry also strives to provide up-to-date information about FA for healthcare professionals, patients and their families.
Patients:
- 300-450 patients
Consent:
- specific consent
Chronic hepatitis B virus infection is currently incurable. Controlling viral replication with reverse transcriptase inhibitors (nucleoside analogues) is possible in over 90% of cases. However, nucleoside analogues have only a very minor effect on cccDNA, the HBV matrix in the nucleus of liver cells. Therefore, the main objective of the overarching DZIF project is to find new concepts for achieving the goal of a cure for HBV.
i.Vacc – individual vaccination
Pioneering individual vaccination
Investigation of multi-omics big data in the population based on a digital mHealth cohort
Further information:
https://www.helmholtz-hzi.de/de/forschung/forschungsprojekte/ansicht/projekt/detail/ivacc-4/
INDIRA – Integrative data analysis for RSV risk assessment
Respiratory syncytial virus (RSV) is the most common cause of severe respiratory disease in young children. Approximately 1% of infections are severe, but risk factors are not well understood. Using multidimensional OMICs data and machine learning methods, the INDIRA joint project identifies genetic markers and biomarkers for the prognosis of severe RSV infections and clarifies their role in the course of infection. In the future, this information will be used for individualised risk assessment and tailored prevention.
Cooperation Prof. Dr. Pietschmann, Twincore Hannover

The influenza study is being conducted in cooperation with TWINCORE and the HZI in Braunschweig.
Following completion of a pilot study with 34 participants, the main study (starting in autumn 2015) will include around 300 participants. Individuals aged 60-80 will be included, as influenza vaccination is recommended for this age group in Germany. Excluded will be (1) individuals with a known allergy to chicken protein, as the vaccine may contain traces of chicken protein, and (2) individuals who, due to limited cognition, cannot fully understand the consequences of participating in the study.
Subjects:
- Pilot: 35 subjects
- Main study: 300 subjects
- Age 60-80 years
2nd funding period of KFO311
The consortium, in which nine clinics and institutes of the MHH conduct joint research, develops treatment strategies and reparative therapies for patients with severe heart and lung diseases. The aim is to further develop mechanical relief and also to identify new reparative therapies that serve to restore the heart and lungs.
With the results of the first funding period, we are well on our way and now want to further develop these approaches into therapies for our patients. The poor prognosis for these patients should improve sustainably, their lives should be prolonged and their quality of life should be improved.
Specifically, in the second funding period, we would like to (i) gain a better understanding of the biological effects of mechanical relief and the pathomechanisms of tissue repair in acute and (pre-)terminal heart and lung failure, (ii) define new reparative therapy approaches in model organisms and translate already identified therapy strategies towards clinical application, and (iii) further develop relief therapy in patients on an evidence-based basis. Structurally, KFO311 combines cardiological, pneumological, cardiac/thoracic surgical and pathological expertise as well as experience in multimodal imaging in the experimental and clinical field at the MHH. KFO311 benefits from its network of excellent associated institutes and the central facilities and core units of the MHH for preclinical research and clinical studies. We also promote young academics in the clinic with structured programmes at the MHH.
Pathology platform for heart and lung tissue and liquid biobanking
In the second funding period, KFO311 benefits from an already established and unique infrastructure for the rapid processing of fresh human tissue and body fluids, as well as biobanking and long-term storage. Quickly available, expert-assessed and extremely valuable tissue from human and animal hearts and lungs, as well as standardised liquid samples, are generated, thus adding value for the research groups belonging to KFO311.
To provide a comprehensive overview of available samples and sample quality, a sample platform is being implemented in which all samples are visible.
Project leaders:
Prof. Dr Thomas Illig
Prof. Dr Danny Jonigk

With 200,000 participants and 18 study centres across Germany, the NAKO health study is the largest health study in German history.
Between 2014 and 2018, a total of 10,000 participants from the greater Hanover area were included in the long-term study at the Hanover study centre. Since December 2018, participants have been invited to the study centre for their second examination.
Further information:
Innovation project for the further development of care following kidney transplantation
further Infomation

PROBASE study
Measuring prostate-specific antigen (PSA) levels in the blood plays an important role in both the diagnosis of prostate cancer – referred to by doctors as prostate carcinoma – and in monitoring prostate cancer treatment. However, its use in early detection is controversial. On the one hand, PSA screening, i.e. the regular measurement of PSA levels in all men above a certain age, allows prostate cancer to be detected earlier and therefore treated more effectively, which reduces mortality. On the other hand, some men with prostate cancer have such a favourable prognosis that they do not necessarily require treatment. However, treatment often begins when prostate cancer is detected. In addition, PSA measurements can produce results that falsely indicate the presence of prostate cancer. For this reason, general PSA screening can lead to further examinations and treatments that are often physically and psychologically stressful and would not have been necessary without screening.
Against this background, men aged 45 and over are currently entitled to reimbursement for an annual digital rectal examination under the statutory health insurance system. PSA testing, on the other hand, is only reimbursed if the man has symptoms that indicate prostate disease. Men who wish to undergo early detection by means of PSA testing must pay for this themselves, as well as any ultrasound examination of the prostate from the intestine, as an individual health service (IGeL).
The PROBASE study (Risk-adapted prostate cancer early detection study based on a ‘baseline’ PSA value in young men – a prospective multicentre randomised trial) is investigating a modern concept for general PSA screening. In this risk-adapted strategy, PSA tests are performed depending on the individual risk of the man, which is determined on the basis of a baseline PSA value at the age of 45 or 50.
Further information:

“REBIRTH active women”
Improvement of endogenous regeneration in female healthy volunteers through physical exercise “REBIRTH active women”
‘REBIRTH active women’ is a study conducted by Hannover Medical School in which female employees between the ages of 45 and 60 took part, provided they had never done any sport before. Around 300 female employees, from nursing managers to laboratory assistants, signed up to exercise for 30 minutes a day. Scientists had already suspected from other studies that exercise keeps you fit. However, no one had expected the effects to be so clear: physical age was reduced by more than ten years within this short period of time.
Study design:
Longitudinal cohort study with randomised control group
Number of subjects:
Approximately 300 subjects
Stored biomaterials:
- Plasma
- Serum
TRAC 19 – Transmission Analysis Covid 19
Lower Saxony school model project to investigate SARS-CoV-2 infection routes among schoolchildren and their teachers over time.
The reopening of schools after the previous complete lockdown, in accordance with the phased plan of the Lower Saxony Ministry of Education and Cultural Affairs, offers a unique opportunity to investigate the prevalence and the expected increased incidence of COVID-19 among children and young people (pupils) with each other and with adults (teaching staff) can be investigated at selected school locations in Hanover. The proposed study will, for the first time, provide quality-assured, up-to-date and, moreover, very rapid (within 6-8 hours) real-time data on the chain of infection and its spread, and thus the essential information for establishing knowledge-based decision-making aids. These important findings will enable appropriate and effective measures to be taken and improved crisis management to be prepared for further cases. This would make Lower Saxony an innovative model location and enable it to provide important information not only for the entire Federal Republic, but also for other highly industrialised societies with a similar age structure and far beyond. The proposed project is an innovative model project for immediate effective support in the fight against SARS-CoV-2 through transdisciplinary and interdisciplinary study cooperation between LUH, MHH, NIFE and HMTMH, which, if implemented, will also lead to international visibility in science and society.
Cooperation partners:
- Gottfried Wilhelm Leibniz University Hannover (LUH)
- Hanover University of Music, Drama and Media (HMTMH)
- Hanover Medical School (MHH), Hanover Unified Biobank (HUB)
- Lower Saxony Centre for Biomedical Engineering, Implant Research and Development (NIFE)
Biomaterial:
- Plasma, buffy coat
Prospective cohort study:
Blood samples will be taken from pupils (5th to 12th grade) at a school, adult family members living in the household (1,000) and teachers (75) and tested for SARS-CoV-2 antibodies and COVID-19. An initial examination will be followed by up to two follow-ups. This will be followed by a statistical analysis of the prevalence and incidence of SARS-CoV-2 infections and the prevalence and incidence of antibodies against SARS-CoV-2 in all groups.
The project may be extended to other schools.
Study investigates the effect of delayed processing of biological samples (blood/urine)
The Q-Map study (Quality Markers to access processing delay) aims to clarify the extent to which delayed processing of blood and urine samples influences subsequent analyses, in particular whether metabolites can be used as markers for such delayed processing (metabolites are metabolic products such as sugars, fats, amino acids, etc.) and whether delayed isolation of blood cells from blood samples, e.g. due to transport times, has an impact on the yield and viability of these cells. Overall, this study serves to continuously improve and test the quality of biomaterials. This is of great importance for future research questions.
20 subjects:
- healthy,
- male
- 20-35 years
- Normal weight according to DGE (body mass index: 20-25)
- No long-term medication, no medication taken in the last 48 hours
- Fasting at the time of the examination (no food or liquids except water for 8 hours beforehand)
Biomaterials:
- Plasma
- PBMCs
- Urine
ZIFCO – Integrated Infection Research Cohort of the German Centre for Infection Research (DZIF) in the NAKO Health Study
The aim of ZIFCO is to use the infrastructure and data generated in the NAKO Health Study for translational infection research in Germany, utilising the latest developments in eHealth.
The ZIFCO study prospectively investigates risk factors for acute infections of the respiratory tract, gastrointestinal tract and urogenital tract, as well as susceptibility to such infections. Conversely, it will also examine the extent to which acute infections and susceptibility to them can be a risk factor for other non-communicable diseases (e.g. cardiovascular diseases).
Further information:
https://www.helmholtz-hzi.de/de/forschung/forschungsprojekte/ansicht/projekt/detail/zifco/
Investigation into the effectiveness of preparatory concepts in the field of stem cell transplantation for rare congenital intestinal diseases.
CAR T-cell therapies at the MHH Haematology Clinic
Chimeric antigen receptor (CAR) T-cell therapy is a
specific cell therapy in which the patient's own (autologous) immune cells are genetically
modified to target and destroy tumour cells. As part of the manufacturing process, the patient's T cells, which are otherwise capable of killing infected
or damaged cells, are equipped with a synthetic
receptor that enables them to recognise cancer cells. This allows the
CAR T cells to specifically attack and kill the cancer cells.
weitere Infos
The paediatric gastroenterology and hepatology department at MHH is part of the international ChilSFree study on immune monitoring after liver transplantation.
Study of paediatric nephrology
Study of paediatric nephrology
Systematic population-based comparison of different home self-examination methods for HPV smears in the context of cervical cancer prevention
Brief description:
Why? Once a year, every woman aged 20 and over with health insurance can visit their gynaecologist for a free preventive examination. In addition to a gynaecological examination, women between the ages of 20 and 34 undergo a cervical smear test (Pap test) to detect cell changes. From the age of 35, testing for human papillomavirus (HPV) is carried out every three years in combination with the Pap smear. These viruses are responsible for almost all cases of cervical cancer and corresponding precancerous lesions. The problem is that 30 per cent of all women in the UK do not regularly take advantage of the statutory early detection programme. One way to reach those who do not want to visit a doctor's office is through an HPV self-testing procedure.
What? The aim of the HaSCo study is to clarify whether a self-test for HPV infection at the cervix could possibly supplement normal screening in the future – especially for women who do not attend regular screening and therefore have an increased risk of developing cervical cancer.
How? In the study, the women are divided into two groups: the first group of 10,000 women will be sent the self-smear test kit with instructions and a questionnaire directly. The second group (also 10,000 women) will first receive an information letter with which they can request a self-smear test kit. The participation rates of the invitation models will be compared later and the CE-certified HPV self-testing systems used will be evaluated. Normal results will be communicated in writing, and further tests will be carried out in the event of abnormal results.
For further information: https://www.mhh.de/hasco-studie
Studie der Pädriatischen Nephrologie
Clinical research
Intellectual disability - General
Krebsprädispositionssyndrom Register
Leukaemia
Immune monitoring during checkpoint therapy
NEKTOR registry study
As part of NEKTOR (Lower Saxony ECT Outcome Registry), patients receiving electroconvulsive therapy (ECT) are recruited.
ear biobank
Psychiatry Psychosis Biobank
REBIRTH active school pilot study: Primary school pupils become more productive and have fewer risk factors for cardiovascular disease
Children and young people need exercise and sport for their physical and mental development. Today, this is clearly lacking in everyday life. Families and schools are often not sufficiently informed about the serious consequences and do not take countermeasures. While around 50 per cent of children are still sufficiently physically active at preschool age, this figure drops dramatically to only 10 per cent by adolescence. There is an urgent need for action here. In the REBIRTH active school pilot study, second-year primary school pupils took part in playful exercise sessions throughout the school day. The study showed significant improvements in physical health and performance, as well as a reduction in risk factors for cardiovascular disease among the participating primary school pupils.
Further links and information
Stigmatisation and depression
Studies by the Central Animal Laboratory
Study of paediatric nephrology
COMBACTE (Combatting Bacterial Resistance in Europe)
Antimicrobial resistance (AMR) is a growing problem worldwide. With few new drugs coming onto the market, there is an urgent need for new antibiotics to treat resistant infections.
The IMI-funded COMBACTE project aims to provide the urgently needed impetus for the development of new antibiotics by pioneering the design and implementation of new approaches for efficient clinical trials in antibiotic development.
COMBACTE is part of the ‘New Drugs for Bad Bugs’ (ND4BB) initiative, the IMI's broad programme to tackle the problem of AMR.
Link:
Samples were collected from CAP and COPD patients at two sites.
Patients:
- 30 CAP patients (12/2015)
- 15 COPD patients (12/2015)
- Controls
Biomaterials:
- EDTA blood
- Plasma
- PAXgene
- Various swabs (nasopharyngeal, groin, oral)
- Stool
- Sputum
- Urine
Consent:
- Specific consent