Hand, foot and rheumatologic surgery
The Upper Extremity, Foot and Rheumatological Surgery Section treats congenital malformations, acquired deformities, injuries, paralysis and chronic diseases of the hands and feet, as well as special changes in rheumatic diseases of the joints, tendon sheaths and bursae.
We use our hands as sensory organs, means of communication and tools to grasp and understand our environment. Just as we have a firm grip on everything with our hands, our feet are the foundation on which the body rests. They enable us to move freely and explore our environment. Functional disorders of the hands and feet significantly impair our quality of life. Social isolation due to lack of movement and the need for care are imminent. Rheumatic diseases are a common cause of functional disorders of the hands and feet. They are caused by the immune system, which is supposed to protect the body against infections and cancer, attacking and destroying the body's own cells. In addition to inflammation of the joints, tendon sheaths and bursae, it can also cause damage to internal organs such as the lungs, liver, intestines, skin, nerves and blood vessels. If medication and conservative treatments do not help sufficiently, surgery is required to prevent or repair damage.
The Upper Extremity, Foot and Rheumatological Surgery Section of the Trauma Surgery Department is your competent partner for the treatment of complex surgical conditions of the hands and feet as well as rheumatic diseases of all joints, tendons and bursae. Many operations can be performed using minimally invasive or arthroscopic techniques. Therapies are constantly being adapted and refined based on the findings of accompanying research. In the case of rheumatic diseases in particular, the correct sequence of operations must be determined individually in order to avoid unnecessary interventions. We advise and treat you individually in order to achieve the best possible result for you.
Hand surgery
All hand surgeries are carried out under modern aspects such as the use of the smallest possible surgical accesses (wounds) with optimum visibility (operation with magnifying glasses). By choosing the most stable osteosyntheses and tendon sutures possible, early functional treatment is carried out wherever possible in order to minimize the risk of movement restrictions and functional disorders. The procedures are constantly being supplemented by useful innovations and improved by the results of accompanying research.
A large proportion of hand surgery procedures are performed on an outpatient basis. Outpatient operations are carried out in a pleasant atmosphere for patients, away from the hustle and bustle of the trauma surgery ward and the main surgery wing.
Due to the complex anatomical conditions (a large number of nerves, tendons, vessels, joints and bones in a very small space), it is absolutely essential for the successful treatment of hand disorders that a treatment plan is drawn up for the patient by the hand surgeon in collaboration with physiotherapists, occupational therapists, the physician in private practice and the patient as equal partners. The best possible treatment result can only be achieved if the follow-up treatment is carried out consistently.
Successful operations on the hand require special knowledge in order to avoid complications [movement restrictions due to scars or ligament shortening (contractures), tearing of fine sutures or screws, etc.]. For this reason, these operations are performed by a hand surgeon at the Department of Trauma Surgery at the MHH.
A particular focus is on the correction of rheumatic wrist and finger deformities. Thanks to the use of modern surgical methods, many cases can now be treated without the use of casts. Early exercise of the joints leads to a faster improvement in movement, stimulates bone healing and enables early skin care.
Wrist arthroscopy is another valuable method of surgical treatment due to the reduced disruption to the patient compared to open surgery. This involves inserting a very thin fiber optic into the various sections of the wrist. The joint capsule, synovial membrane, ligaments, free joint bodies, cartilage and the triangular disc can thus be viewed directly, examined with fine instruments and treated in the same operation. Arthroscopically assisted partial arthrodeses can restore the stability of the wrist without severely disrupting the circulation. Not only are the scars smaller, but the bone also heals faster and more reliably. As the wrist can be moved unhindered in a special holding device developed in our department, functional disorders can be detected that can escape X-ray examination as well as computer tomography (CT) and magnetic resonance imaging (MRI). Although the majority of pathological changes found can be treated arthroscopically, open surgery may still be necessary in many cases to treat complaints.
- Hand injuries
- Correction of damage resulting from accidents [healing in incorrect position, incorrect growth after childhood accident, lack of bone healing (pseudarthrosis), functional impairments due to scars, restricted joint movement]
- Growth control for congenital and acquired malpositions in the growth phase
- Arthrosis [hand, thumb saddle (rhizarthrosis), finger joints (Heberden/Bouchard arthrosis)]
- Elimination of finger, hand and elbow joint pain (denervation) for severe finger and wrist wear, tennis and golfer's elbow
- Rheumatic hand deformity (restoration/improvement of hand function through soft tissue and bone stabilizing corrections, finger joint replacement, tendon restoration)
- Therapeutic wrist arthroscopy [cartilage smoothing, synovial membrane removal (synovialectomy), arthroscopically assisted partial wrist fusion and resection of diseased bones (minimally invasive surgery), operations on the triangular disc (TFCC), removal of free joint bodies]
- Dupuytren's disease
- Therapy-resistant tendon sheath inflammation (tendovaginitis stenosans, rapid finger, rheumatic diseases)
- Restoration of hand function in cases of paralysis due to injury, after a stroke or in the context of neurological diseases
- Nerve pain and nerve bottleneck syndromes (neurolysis, carpal tunnel syndrome, sulcus ulnaris syndrome, etc.)
- Tumors of the hand
- Congenital malformations
- instructions for physiotherapeutic exercises to maintain independence
- occupational therapy, including the provision of aids
- prescriptions for splints (ortheses)
- injections and infiltrations
- chirotherapy
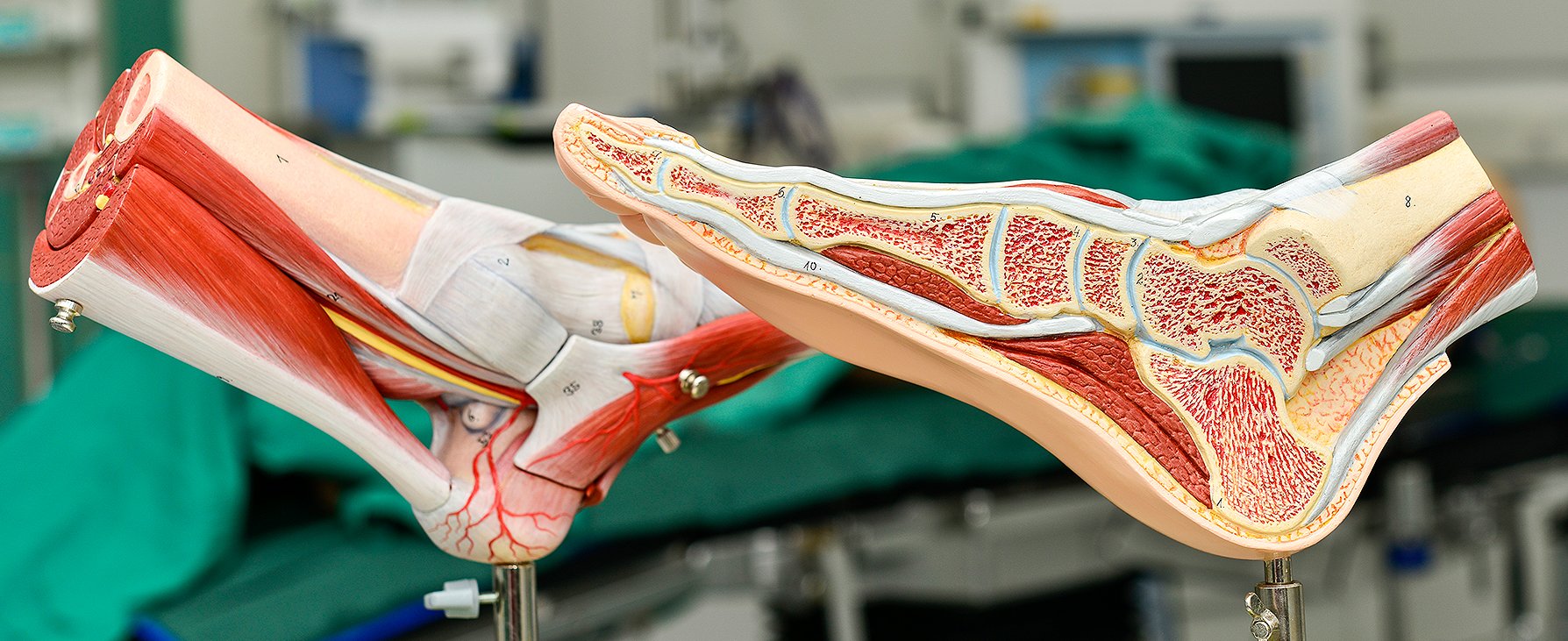
Foot surgery
All foot surgery operations are carried out under modern aspects such as the use of the smallest possible surgical accesses (wounds) with optimum visibility (operation with magnifying glasses). By choosing the most stable osteosynthesis procedures and tendon sutures possible, early functional treatment is carried out wherever possible in order to minimize the risk of movement restrictions and functional disorders. The procedures are constantly being supplemented by sensible innovations and improved by the results of accompanying research.
Some foot surgery is performed on an outpatient basis. Outpatient foot operations are carried out in a pleasant atmosphere for patients, away from the hectic pace of trauma surgery wards and the main operations tract.
Due to the complex anatomical conditions (a large number of nerves, tendons, vessels, joints and bones in a very small space) and the poor circulation of the feet, it is absolutely essential for the successful treatment of foot disorders that a treatment plan is drawn up for the patient by the foot surgeon in collaboration with physiotherapists, orthopaedic shoe technicians, practising physicians and the patient as equal partners. The best possible treatment result can only be achieved if the follow-up treatment is carried out consistently.
Successful operations on the foot require special knowledge in order to avoid complications (movement restrictions due to scars or ligament shortening [contractures], tearing of fine sutures or screws, etc.). For this reason, these operations are performed by a foot surgeon certified by the German Association for Foot and Ankle Surgery (D.A.F.).
A particular focus is on the correction of rheumatic ankle, hindfoot and forefoot deformities. The aim of this therapy is a fully weight-bearing, pain-free foot with the greatest possible stability and mobility. The corrected foot should fit back into a normal shoe (ready-made shoe), thus avoiding the need to wear orthopaedic shoes. Today, orthopaedic shoes should only be used in exceptional cases, as they are very heavy and put a lot of strain on the other joints of the legs, including the spine.
Arthroscopy can be used to examine the upper ankle joint in particular under direct vision while moving in order to detect pathological changes (ligament instability, cartilage damage). In the case of osteoarthritis of the upper ankle joint, mobility can be improved by arthroscopic removal of bone growths (osteophytes). Free joint bodies and folds in the synovial membrane (synovium), which destroy the cartilage by pinching, can also be removed arthroscopically. In the case of rheumatic diseases, joint suppuration (empyema) or crystal deposits (chondromatosis and gout), the synovial membrane can be removed minimally invasively using special instruments. Arthroscopy is also used to drill holes in osteochondrosis dissecans to prevent cartilage damage. In selected cases, minimally invasive arthroscopic fusion of the upper ankle joint is also performed.
The diabetic foot, which was previously considered inoperable and was generally treated in an orthopaedic shoe, can now be corrected in many cases thanks to new stable-angle implants and gentle surgical techniques so that normal footwear can be worn with a diabetic footbed. The bone heals much more slowly in diabetics due to the circulatory disorder, which is why longer periods of immobilization or partial weight-bearing are required. Modern lightweight plastic orthoses can usually be used without a cast, which facilitates mobilization after the operation.
Neurological diseases can lead to deformation due to spasticity or flaccid paralysis, resulting in incorrect weight-bearing or even inability to put weight on the feet. The reduction in sensation and the reduction in the weight-bearing zone leads to ulceration with pain and the risk of deep infection, which can lead to the loss of the foot. As the knee and hip joints are often affected as well as the feet, a thorough examination of the whole body is carried out before the operation, followed by the planning of the necessary conservative and surgical steps. In many cases, the ability to walk can be maintained or restored through complex positional corrections.
Stabilization of unstable joints is initially attempted conservatively through physiotherapeutic muscle strengthening and reflex training (proprioceptive training). If these fail, plastic ligament surgery is used; in rare cases, stabilization can only be treated safely by fusion (arthrodesis) if wear has already occurred.
In contrast to the hip and knee joints, prostheses of the upper ankle joint are only indicated in special cases due to the high complication rate, but can lead to good results. Prostheses of other ankle joints are not recommended due to very poor results. Alternative therapies involving stiffening (arthrodesis) or joint removal (resection arthroplasty) are (still) preferred.
- Foot injuries
- Correction of damage resulting from accidents [healing in the wrong position, lack of bone healing (pseudarthrosis), functional impairments due to scars, restricted joint movement]
- Osteoarthritis treatment of the upper ankle joint, tarsal and toe joints
- Correction and growth control of congenital and acquired deformities of the upper ankle joint, tarsus and toes (fallen arches, splayfoot, clubfoot, hallux valgus, claw toes, etc.)
- Correction of paralyzed feet to maintain and restore the ability to walk
- Correction of rheumatic foot deformities (restoration of a weight-bearing foot, avoidance of heavy orthopaedic shoes)
- Therapeutic arthroscopy of the upper ankle joint [cartilage smoothing, removal of synovial membrane (synovialectomy), removal of bone braces (osteophytes), removal of free joint bodies, fusion (arthrodesis)]
- Tendon surgery [Achilles tendon pain, peroneal tendon dislocations, restoration of foot elevation through tendon displacement (stirrup plasty), etc.]
- Ligament plastic surgery to stabilize the upper and lower ankle joint
- Tendinitis resistant to therapy
- Nerve bottleneck syndromes (tarsal tunnel syndrome, etc.)
- Tumors of the foot
- Diabetic foot
- Septic (inflamed) foot
- Endoprosthetic replacement of the upper ankle joint
- Correction of congenital malformations
- Instructions for physiotherapeutic exercises
- Prescriptions for insole fitting and shoe fitting
- Prescriptions for splint fitting (orthoses)
- Injections and infiltrations
- chirotherapy
Rheumatism orthopaedics
All rheumatoid orthopaedic operations are carried out under modern aspects such as the use of the smallest possible surgical accesses (wounds) and the most stable possible osteosyntheses and prostheses, whereby the procedures are constantly supplemented by sensible innovations and improved by the results of accompanying research. Many operations on the shoulder, elbow, hand, hip, knee and upper ankle joints are carried out using arthroscopy in order to enable faster recovery through a gentle surgical approach.
But the rheumatism orthopaedist can do more than just operate! In addition to necessary operations, alternative procedures such as the optimization of drug therapy (in cooperation with the rheumatologist), physiotherapy, occupational therapy, splints (orthoses), insoles and shoes or injection treatments (injections) and synoviortheses are always discussed with the patient at every presentation in the rheumatism orthopaedic consultation. Wherever possible, surgery should only be performed if non-surgical treatment methods have been unsuccessful or do not promise success.
In order to treat rheumatic diseases effectively, it is essential that a treatment plan is drawn up for the patient by the rheumatologist orthopaedist in collaboration with an internal medicine rheumatologist and the patient as equal partners. If the symptoms change, this plan must always be adapted to the current symptoms in order to enable optimal treatment.
Successful operations on rheumatism patients require special knowledge in order to avoid complications, especially due to the side effects of the very effective new drugs (biologicals, e.g. TNF-α receptor antagonists, etc.). For this reason, these operations are performed by a rheumatology orthopaedist at the MHH's Trauma Surgery Department. Close cooperation with the internal rheumatologists at the MHH also ensures that drug therapy is optimized.
The special focus is on the correction of rheumatic wrist and finger deformities, which must be considered together and treated in the correct order for successful correction. Thanks to the use of modern surgical methods, many cases can now be treated without heavy and uncomfortable casts, which minimizes the risk of cast pressure points, restricted movement and an increase in osteoporosis. Early exercise leads to improved joint mobility and faster bone healing. Skin care is possible at an early stage thanks to light, removable splints or often even splint-free follow-up treatment. The aim of treatment is to restore the best possible function of the hand and thus maintain or regain independence (e.g. personal hygiene, housework, work and sport).
As with the hand, the correction of rheumatic foot deformities, which is another key area, requires the correct sequence of correction to achieve the desired result. In addition, rheumatic feet often require a different operation in order to achieve the best possible result, even if the external aspect of the deformity is similar to that of non-rheumatic patients (e.g. hallux valgus, claw toes, bowed foot, flat foot, splayfoot). The aim of treatment here is to restore pain-free walking and to make it easier to wear shoes in order to maintain or regain independence (e.g: Pain-free walking inside and outside the home, wearing normal footwear with insoles instead of heavy orthopaedic shoes)
Joint replacement (endoprosthesis) on the hip, knee, shoulder, elbow, fingers and upper ankle joint, including complex endoprosthesis replacement in the event of prosthesis loosening, fracture, instability (repeated dislocation) and infection, is the third focus of rheumatic orthopaedic care. Here, too, the procedures for rheumatics are more demanding than for osteoarthritis due to the additional need for thorough removal of the synovial membrane (synovialectomy). In addition, the bone is very soft due to osteoporosis and the leg axis misalignments (knock knees and bow legs) are often more pronounced and therefore require more correction in order to maintain a straight leg axis. If treatment with a standard prosthesis is no longer possible due to bone loss or destruction of the soft tissue caused by the rheumatic inflammation, individual or multi-part (modular) prostheses are used. The aim of treatment is to improve or restore joint function (e.g. pain-free walking with straight legs, stabilization of dislocated and unstable joints).
The fourth focus is the minimally invasive removal of the synovial membrane under visualization with a fibre optic camera (arthroscopic synovialectomy). This procedure has largely replaced open surgery on the shoulder, elbow, knee and upper ankle. Although arthroscopic synovialectomy can be used well on the wrist, it is often performed openly due to the need to remove the tendon sheath at the same time, which is an open operation. The aim of the treatment is to relieve pain and preserve the patient's own joints and tendons. If the synovial membrane is removed in good time, joint destruction can be slowed down and the use of an endoprosthesis delayed. Removing the tendon sheaths prevents tendon destruction caused by the inflamed tissue and thus helps to avoid costly tendon replacement operations.
- Arthroscopy of the shoulder, elbow, hand, hip, knee and upper ankle joint
- Open joint-preserving operations
- Restoration of rheumatically damaged tendons and ligaments
- Stabilizing operations on unstable joints (loose joints)
- Joint replacement (endoprostheses) on the shoulder, elbow, finger, hip, knee and upper ankle joint for rheumatic joint destruction with correction of the leg axis (X- and O-leg malalignment)
- Removal of inflamed synovial membrane, tendon sheaths, bursae and rheumatoid nodules
- Correction of rheumatic wrist and finger deformities (hand scoliosis, buttonhole deformity, swan-neck deformity of the II-V finger, 90-90 deformity of the thumb, etc.)
- Correction of rheumatic foot deformities (bowed foot, flat foot, splayfoot, hallux valgus, etc.)
- Relief (neurolysis) and relocation of pinched nerves (e.g. carpal tunnel syndrome, ulnar sulcus syndrome, tarsal tunnel syndrome, etc.)
- Elimination of finger, hand and elbow joint pain (denervation) (e.g. tennis elbow, golfer's elbow, osteoarthritis)
- Injuries (accidents) and consequences of injuries in rheumatics
- Instructions for physiotherapeutic exercises to maintain independence
- Physiotherapeutic exercise treatment
- Occupational therapy including provision of aids (helping hand, raised toilet seat, etc.)
- Splint care (orthoses)
- Prescriptions for insoles, orthopaedic shoe fitting
- Injections and infiltrations
- Chirotherapy
The preparation of therapy plans, optimization of drug and physical therapy is carried out in close cooperation with your treating internal rheumatologist and/or the Department of Rheumatology and Immunology at the MHH, your occupational and physiotherapist and/or the Clinic for Physical Therapy and Rehabilitation at the MHH as well as the Pain Outpatient Clinic of the Clinic for Anaesthesia and Intensive Care Medicine at the MHH.
Important information
For best results, please bring the following with you:
- List of all known illnesses
- List of all previous operations (with date and hospital or practice, operation report)
- all available X-ray, CT and MRI images (preferably on CD-ROM)
- All existing aids (insoles, splints, fitted and orthopaedic shoes, bandages)
- Referral from a surgeon, orthopaedist or rheumatologist to "MHH Unfallchirurgie"
Attention:
As the hand, foot and rheumatism consultation is very busy due to the high demand, you should expect to wait several hours, so please bring provisions and reading material with you.