Anatomy
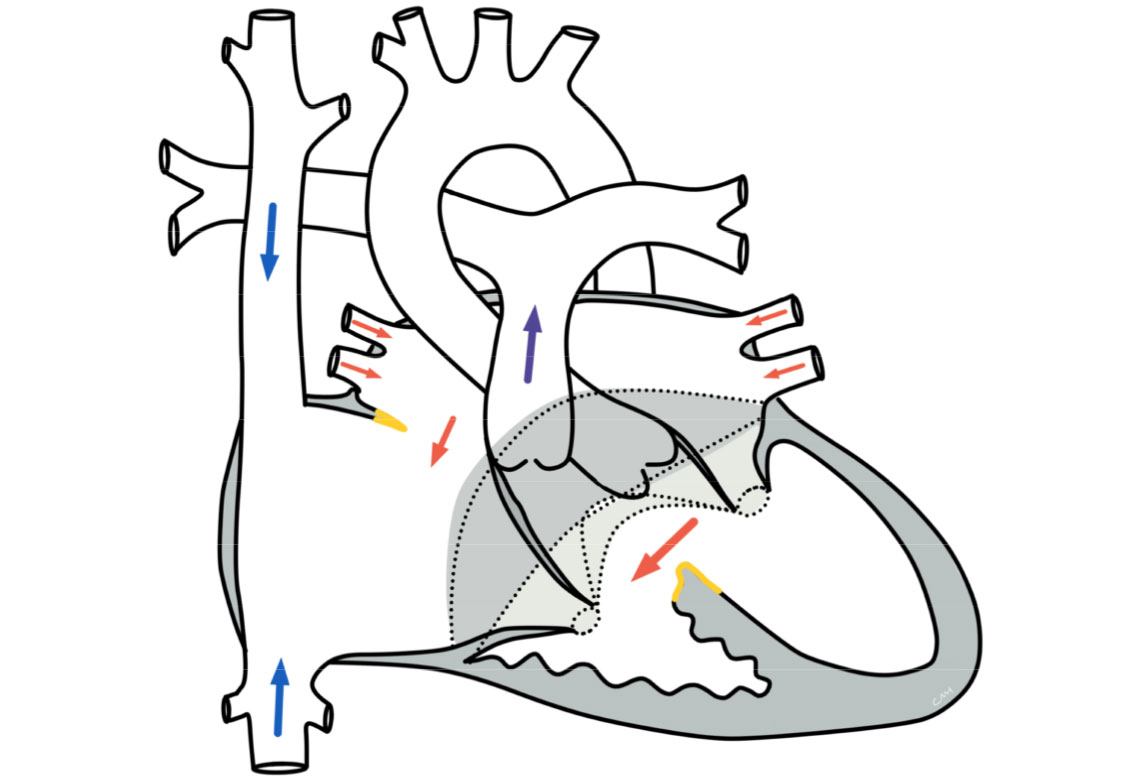
There is a combination of several defects, which can be present in varying degrees and also only partially:
- Ventricular septal defect (VSD): Gap in the inlet portion of the ventricular septum
- Atrial septal defect (ASD): Gap in the lower portion of the atrial septum (septum primum)
- Complex anomaly of the atriventricular heart valves (AV valves) between the atria and ventricles: The valve ring and the connective tissue leaflets are malformed, there may be various manifestations and degrees of severity. As a rule, there is a common valve ring with varying degrees of formation of the valve leaflets (usually 5 leaflets). The suspension of the valve parts by their retaining cords is often malformed.
Physiology and hemodynamics
The septal defects at the atrial and ventricular level lead to a mixing of blood from the systemic and pulmonary circulation, usually to a directed flow from the left to the right side of the heart (so-called left-to-right shunt). This results in a volume load on the left heart and lungs. In the case of large defects in the ventricular septum, pressure equalization of the right and left ventricle occurs. This can lead to the development of pulmonary hypertension. This results in increased pressure in the blood vessels of the lungs, which can lead to severe vascular and tissue damage to the lungs if left untreated.
In so-called partial AVSD, the septal defect is only present at the level of the atria(see ASD I).
If the right and left halves of the heart are significantly different in size due to the blood flow conditions, this is referred to as an imbalanced AVSD.
Treatment of an atrioventricular septal defect
Conservative stabilization
In the treatment of AVSD, total surgical correction is the treatment of choice in the first few months of life. The aim is to create normal anatomical conditions for the heart. However, this surgical option may not be available in cases of particularly severe AVSD (so-called imbalanced form) or other accompanying circumstances (prematurity, other cardiac anomalies, other organ malformations).
With AVSD, there is often an imbalance in blood distribution to the detriment of the lungs (pulmonary hypertension). This can lead to pulmonary hypertension on the one hand and cardiac insufficiency on the other. These manifest themselves in children through reduced physical resilience, accelerated breathing, excessive sweating and failure to thrive, among other things. For this reason, drug therapy is usually necessary. The medication often has to be continued for several months after the operation.
Surgical therapy
The intended primary surgical total correction is usually performed between the 3rd and 6th month of life and must be carried out with the aid of a heart-lung machine. The septal defects in the atrium and ventricle are closed with one or more tissue patches. By sewing in the patch, the two AV valves are divided. In addition, the individual valve sections are then gathered using a suture technique and leaks are closed.
If the desired total correction is not possible due to concomitant circumstances (e.g. imbalanced AVSD, premature birth, other heart or organ malformations), so-called palliative operations may have to be performed. These include pulmonary artery banding (PAB): This involves placing a belt-shaped loop around the pulmonary artery - with the aim of restricting blood flow into the lungs. The aim is to prevent pulmonary flooding and the development of pulmonary hypertension. This surgical procedure is mainly used to bridge the gap for a later planned total corrective operation.
If there is a very imbalanced variant of AVSD with differently sized ventricles, it may not be possible to correct the heart defect completely by surgery. In this case, alternative, palliative (i.e. alleviating, non-healing) surgical procedures must be used. For example, univentricular palliation can be performed using Fontan circulation (single-chamber heart with passive pulmonary circulation).
Prognosis of an atrioventricular septal defect
Further course
Surgical correction of the AVSD is one of today's standard surgical procedures, although it is often challenging due to the complexity of the heart defect. The postoperative course depends primarily on the reconstruction of the AV valves and their functionality (tightness, opening area).
Furthermore, after AVSD correction there is an increased risk of cardiac arrhythmia postoperatively due to the anatomical conditions. These are often only significant in the first few days after the operation and do not require long-term therapy. More serious residual defects after surgery can become symptomatic later on. For some patients (15 - 20%), further operations are therefore necessary in the course of their lives.
After successful correction, life expectancy is comparable to that of the normal population, and patients should be able to go about their daily lives without restrictions, although they may be limited in their ability to exercise.
Several operations are usually necessary following palliative surgery. A normal life expectancy and full athletic capacity can often not be achieved.
