Dear patients,
If your kidneys finally lose their function, you will have to be treated permanently with an artificial organ replacement procedure (haemodialysis, haemofiltration, peritoneal dialysis). A kidney transplant is a good alternative. It improves your quality of life and can extend your life expectancy.
When you visit the transplant outpatient clinic, experienced transplant physicians will carefully assess your health situation in preparation for the transplant.
Kidney transplants have been performed at the Transplant Centre Hannover since the early 1970s - both with donor organs from deceased and living donors. This also includes living donations with dissimilar blood groups (AB0-incompatible).
The transplant preparation department is constantly looking after around 1,400 patients at various waiting stages.
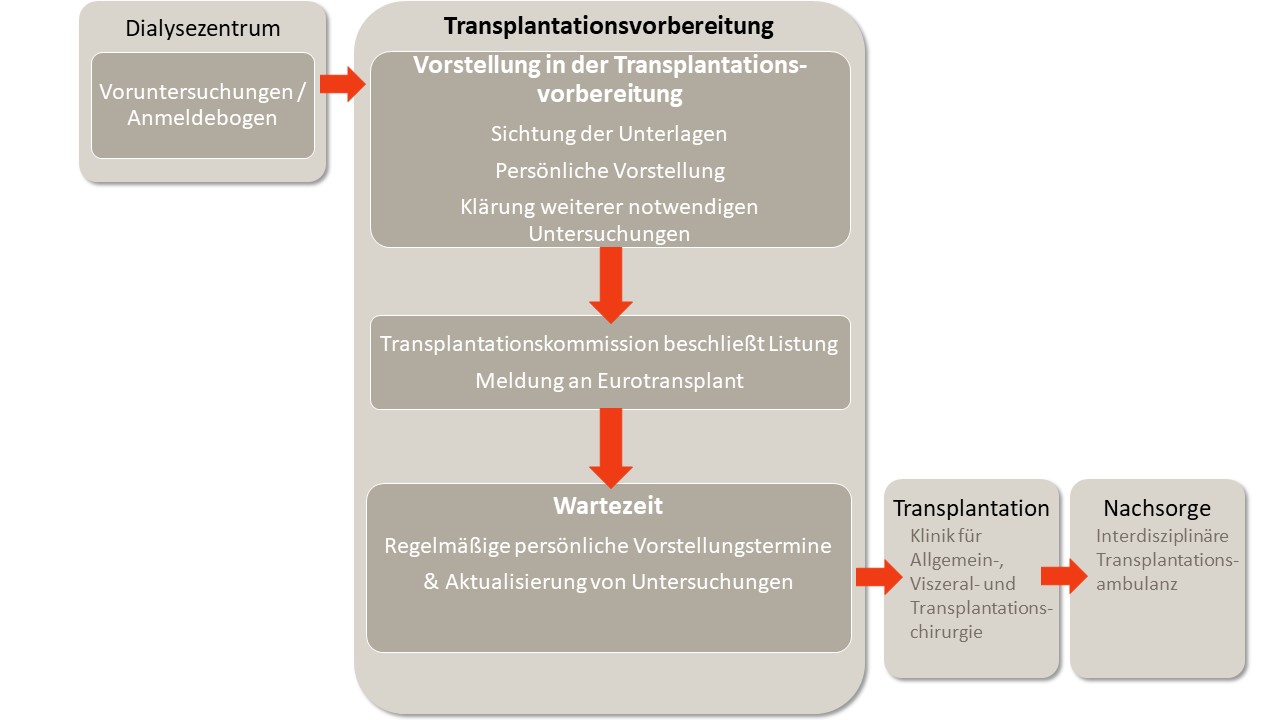
The following diagram provides an overview of the process from registration for a kidney transplant to transplantation.
Transplant registration procedure
Further information
Before you present yourself to us in the outpatient clinic, your nephrologist will carry out some preliminary examinations. Once the preliminary examinations have been completed, the examination results and the registration form must be sent to the transplant preparation department. Once we have received your documents, we will invite you to an initial appointment.
In an initial personal interview, you will have the opportunity to clarify questions, receive information on the procedures and, if necessary, be asked to submit additional findings. At this stage of transplant preparation, you are not yet registered with Eurotransplant. Around a third of the 1,400 patients in the transplant preparation phase are at this early stage of clarification.
If we come to the conclusion based on the findings that you meet the medical requirements for a transplant, your case will be presented to the interdisciplinary transplant commission of the MHH. The commission consists of at least three physicians from nephrology, transplant surgery, transfusion medicine and forensic medicine (representative of the medical director). This committee decides on your registration with Eurotransplant.
The notification of the waiting stage at Eurotransplant can be:
1. "Transplantable (T)": You are suitable for a transplant. In principle, you would be willing to accept an organ offer at any time. Approximately 50 percent of patients undergoing transplant preparation are registered with Eurotransplant as "Transplantable".
2. "Non-transplantable (NT)": According to medical assessment, you are not (yet) suitable to receive an organ offer from a medical point of view (e.g. infection) or you do not wish to accept an organ offer at the moment for personal reasons (e.g. absence on vacation). Approximately 15 percent of the patients cared for in transplant preparation are at the "non-transplantable" waiting level.
In Germany, there are more patients waiting for a kidney than there are donor organs available. The resulting waiting time can be less than five, but also up to ten years. In some special programs, such as the "Eurotransplant Senior Program" ("Old for Old"), the average waiting time is shorter. Certain blood groups (e.g. 0 or B) or the presence of antibodies in the blood can lead to longer waiting times.
The waiting time is calculated on the basis of the first dialysis date. Times at the "non-transplantable" waiting level are included in the calculation of the waiting time (for exceptions, see "Special features of the pancreas/kidney combination listing").
During the waiting period, personal re-presentations take place at regular intervals in the transplant outpatient clinic. Based on your personal impression and updated findings, your suitability for transplantation will be continuously assessed. If your medical or personal situation makes it necessary, your waiting level can be changed at any time from "transplantable" to "non-transplantable" and vice versa.
As soon as you have been transplanted, further care and aftercare will be provided by the Interdisciplinary Transplant Outpatient Clinic of the MHH. You will have to present yourself here in person at regular intervals, for example to check the function of the transplant and adjust the medication.
- This form of combination listing can only be used if an absolute insulin deficiency (diabetes mellitus type 1) has been proven. Proof of this must be submitted to us as a copy of an original laboratory result (fasting C-peptide determination with simultaneous blood glucose determination (for normoglycemia) or alternatively: antibody diagnostics (IA-2, ICA, GAD- ZnT8)).
- Registration can take place before the start of dialysis (from limited kidney function with an eGFR below 30ml/min).
- The waiting time is only calculated from the time of listing with Eurotransplant at waiting level "Transplantable.
- The waiting time can be less than five years.
- Since the Eurotransplant guideline amendment of September 12, 2023, the following applies to the "non-transplantable" waiting level for the pancreas/kidney combination listing:
- If a change of registration becomes necessary for medical reasons, the Transplant Centre can submit an application for the waiting time to be taken into account.
- In the case of vacation periods, this option does not apply, i.e. only times at the "transplantable" waiting level are included in the calculation of the waiting time. - For this form of combination listing in particular, a BMI of max. 27 kg/m² is a prerequisite for listing
.
Here you can find information on Living donation preparation at the Hannover Medical School. The preparation and, if necessary, execution of a living donation can also be started without the need for dialysis.
Questions & answers on other important topics
1. alcohol: It is recommended to abstain from alcoholic beverages. If alcohol is nevertheless consumed, large amounts of alcohol and binge drinking should be avoided.
For patients
Specialist literature
- Position paper of the German Nutrition Society (DGE, from 08/2024)
2. tobacco consumption: It is recommended to refrain from smoking. There is an increased risk of peri- and postoperative infection under immunosuppression as well as the risk of progressive vascular calcification, which may make graft connection difficult or even impossible.
For patients
- www.gesundheitsinformation.de/wo-finde-ich-unterstuetzung-fuer-den-rauchstopp
Specialist literature:
- Pamminger, M., Mayr, A. Cardiovascular consequences of smoking Radiology 62, 763-771 (2022).
- Kasiske, B. L., & Klinger, D. (2000). Cigarette smoking in renal transplant recipients. Journal of the American Society of Nephrology, 11(4), 753-759.
3. cannabis: It is recommended not to smoke cigarettes containing cannabis (inhaled consumption). There are frequent interactions with immunosuppressants, which in turn can increase the risk of rejection. Special feature for oral intake: Individual concepts must be defined before listing with regard to cannabis-containing oral medication (e.g. in the context of epilepsy treatments).
For patients
- cannibo.de/blog/cannabis-and-the-potentially-occurring-interactions-with-polymedication
Specialist literature
- Rodríguez-Ramírez, S., Tang, E., Li, Y., Famure, O., Mucsi, I., & Kim, S. J. (2024). Cannabis use is associated with reduced access to kidney transplantation and an increased risk of acute rejection post-transplant. Clinical Transplantation, 38(2), e15264.
- Kidney transplantation in adults: Evaluation of the potential kidney transplant recipient. Literature review current through: Jan 2025. This topic last updated: Oct 14, 2024. In: UpToDate, Connor RF (Ed), Wolters Kluwer.
Last update: Dr. R. Hanna, March 2025
Pregnancy after kidney transplantation is possible. However, certain individual factors must be taken into account. We generally advise against pregnancy within the first year after transplantation, and stable graft function should be present, preferably with a GFR above 40 mL/min. Another prerequisite is well-controlled blood pressure.
Ideally, we advise couples who wish to have children together about the particularities of pregnancy after kidney transplantation. Such a consultation includes information on menstruation, contraception and previous pregnancies or miscarriages. Important topics include the reduced conception rate, increased miscarriage rate and the risk of pre-eclampsia, eclampsia and other complications such as premature birth and low birth weight. In some cases, direct contact is made with a fertility clinic.
Immunosuppressants must be adjusted before pregnancy, e.g. switching from Cellcept/Myforttic or mTOR inhibitors (Serolimus, Evrolimus) to Azathioprine. Certain blood pressure medications and other therapies may also need to be discontinued or replaced with medications that are permitted during pregnancy.
Regular examinations during pregnancy include blood pressure checks, creatinine measurements, urine analyses and tests for infections, as well as ultrasound examinations of the transplanted kidney. If the pregnancy is complicated, we often work together with a specialized obstetric outpatient clinic (prenatal medicine at the MHH).
In the event of pre-eclampsia, poorly controllable high blood pressure or a deterioration in kidney function during pregnancy, admission to hospital may be necessary.
Last update: Dr. R. Hanna, March 2025
Can we still have children after my fiancé has had a transplant or should we freeze sperm beforehand if I am not pregnant by then? I know that immunosuppressants increase the risk of malformations and premature births and that they can have a negative effect on sperm.
Yes, immunosuppressants could increase the risk of malformations and premature births. There is a so-called"red hand letter" regarding immunosuppressants such as MMF (Cellcept/Myfortic). Animal experiments have shown a negative influence on sperm. If a male patient wishes to have children, we therefore recommend changing the immunosuppression 3 months before and until the onset of pregnancy (conception) (azathioprine would be given instead of Cellcept/Myfortic). This change in immunosuppression is possible without any great risk to the transplant.
Last update: Dr. R. Hanna, March 2025