13.12.2023
Neurooncology update 2023

The Neurooncology Center hosted the annual Neurooncology Update on 13.12.2023.
Program:
17:00 - 17:05 Welcoming remarks Prof. Dr. med. Joachim K. Krauss, Head of the Neurooncology Center
17:05 - 17:25 Significance & function of IDH mutations in gliomas, Prof. Dr. med. Christian Hartmann, Chair of Neuropathology, Institute of Pathology, MHH
17:25 - 17:45 New therapy options for IDH-mutated low-grade gliomas, PD Dr. med. Philipp Schwenkenbecher, Clinical Department of Neurology, MHH
17:45 - 18:05 The polysialicacid-siglecsignaling axis regulates the activation of tumor-associated macrophages in glioblastomas, Dr. med. Hauke Thiesler, Institute of Clinical Biochemistry, MHH
18:05 - 18:25 Identification of new biomarkers as a new diagnostic criterion in malignant gliomas, Dr. med. Nora Möhn, Clinical Department of Neurology, MHH
18:25 - 18:50 BREAK
18:50 - 19:10 The neurosurgical instruments for gliomas: An update on intraoperative technologies to improve safety and extent of resection, Dr. med. Manolis Polemikos, Clinical Department of Neurosurgery, MHH
19:10 - 19:30 Radiotherapy of brain tumors: new developments, Dr. med. Roland Merten, Clinical Department of Radiotherapy and Special Oncology, MHH
19:30 - 19:50 Integrated neuro-oncological aftercare in neurorehabilitation, Dr. med. Markus Ebke, Neurological Early Rehabilitation, Clinical Department of Neurology and Clinical Neurophysiology, DIAKOVERE Henriettenstift
19:50 - 20:00 Discussion Speakers and Chairmen & Closing remarks Prof. Dr. med. Joachim K. Krauss, Clinical Department of Neurosurgery, MHH
The event took place as a hybrid event: the speakers were in lecture hall M with 50 participants and a further 30 people were able to participate online via the dial-in link. All participants - whether online or on site - had the opportunity to ask questions.
December 2023
Dr. med. Florian Wild appointed organ donation advisor at the MHH

Dr. med. Florian Wild, Senior Physician at the Clinical Department of Neurosurgery and Head of the Intensive Care Unit, is the new organ donation consultant at the MHH.
Dr. med. Elvis Hermann, Deputy Director of the Clinical Department of Neurosurgery, remains an organ donation consultant.
11.11.2023
Clinical Department of Neurosurgery presents itself at the MHH Open Day
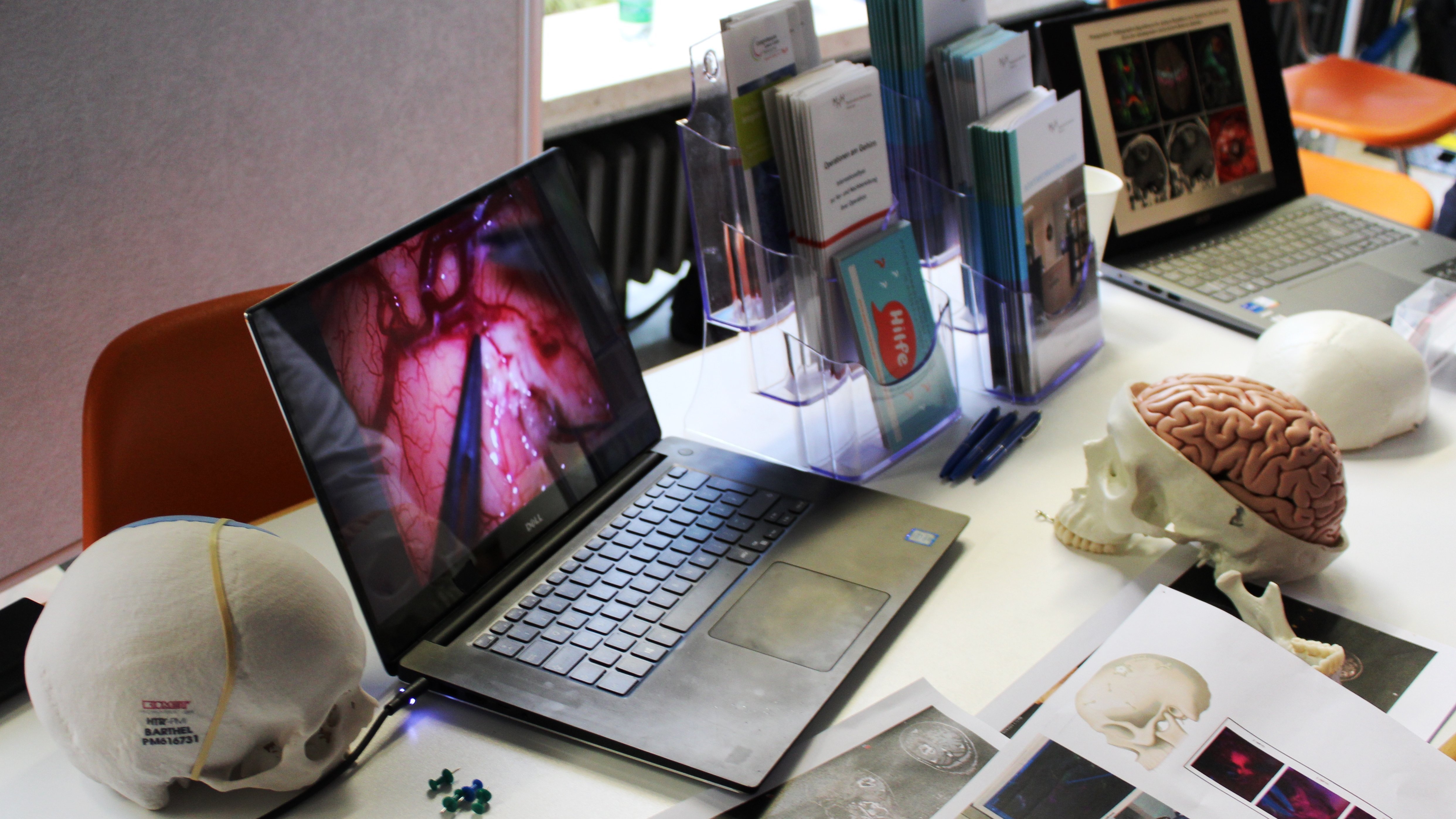
At the Open Day, the Clinical Department of Neurosurgery presented itself together with other clinics and Facilities or Institutions on the Street of Cancer Medicine - The Comprehensive Cancer Center Hannover.
Mr. Genis Bajgora, Assistant Physician at the Clinical Department of Neurosurgery, and Dr. med. Ariyan Pirayesh, Senior Physician at the Clinical Department of Neurosurgery, showed videos of a neurosurgical operation at the "Neurooncology Center: At the center of the nervous system" stand and answered questions from interested participants.
Further information can be found in the MHH-Info issue December 2023 from page 34.
You can also find further information on the invitation here.
04.11.2023
1st Hanover Hands-On Course Neurosurgery for Students

The 1st Hanover Hands-on Neurosurgery Course, organized by the Connectome Students Association for Neurosurgery, Neurology and Neurosciences e.V. and the Clinical Department of Neurosurgery, took place on 04 November 2023. Over 100 students had registered for the event, of which only 50 were able to take part.
The selected students were divided into four groups and went through the various workshops on a fixed schedule.
In the opening ceremony, the organizers spoke
Marcel R. Oelerich (medical student and PhD student at the Clinical Department of Neurosurgery/ MHH), Prof. Joachim K. Krauss, Director of the Clinical Department of Neurosurgery/ MHH (right in the picture) and Mr. Filipe Wolff Fernandes (resident at the Clinical Department of Neurosurgery/ MHH) (left in the picture).
Prof. Joachim K. Krauss gave a lecture on the neuroanatomy and neurophysiology of the basal ganglia to the entire auditorium. Afterwards, Mr. Wolff Fernandes demonstrated the morphology of the basal ganglia with the assistance of the 3D Mixed Reality Viewer from Brainlab.
In addition to the workshops, the coffee breaks allowed for discussions between physicians and students.
14.10.2023
Poster prize for Dr. Manolis Polemikos

Dr. Manolis Polemikos, Senior Physician at the Clinical Department of Neurosurgery, won the second poster prize for the poster entitled "Falcotentorial meningiomas: clinical outcome and volumetric follow-up after microsurgical resection" at the "30th Annual Meeting of the Society of Skull Base Surgery - Next Generation Interventions Overcoming Boundaries in Skull Base Surgery", which took place from 11.10.-14.10.2023 in Hanover. The poster prize is endowed with €500.
12.10.2023
Re-certification Neurooncology Center
The Neurooncology Center of the Hannover Medical School under the direction of Prof. Dr. med. Joachim K. Krauss was recertified by the DKG Cancer Society until 08.05.2026 as part of an online certification (on-site certification did not take place this year).
Neuro-oncology center with recommendation of the German Cancer Society e.V.
10.10.2023
Second meeting of the Neurooncology Working Group

In October 2023, the CCC-N neuro-oncology working group met for the second exchange at the University Medical Center Göttingen.
The central topic of the meeting was the planning of joint clinical studies. Initially, mainly retrospective analyses were discussed, but prospective studies are also already being planned jointly.
Various study ideas were presented by both sites and discussed under the following aspects:
- How should the patient collective be defined?
- How many joint patients would be available for the projects based on experience?
- How should the further implementation take place, who has already done the preliminary organizational work?
The various specialist disciplines present took part in the discussion: Neurosurgery, Neuropathology, Neurology, Oncology and Radiotherapy. In addition to the technical discussions, administrative and regulatory conditions for the concrete implementation of the projects were also discussed with the head of the UMG study center, Ralf Tostmann. The working group meets every six months. The next meeting is planned for spring 2024 at Hannover Medical School.
October 2023
Prof. Krauss is an Editorial Board Member of the Journal of Neural Transmission
Prof. Krauss will be a member of the Editorial Board of the Journal of Neural Transmission from January 2024.
September 2023
Poster Prize ESSFN, 25th Annual Meeting in Stockholm

Mr. Marcel Oelerich, student at the MHH and doctoral student of Prof. Schwabe and Prof. Krauss, won a poster prize at the congress of the European Society for Stereotactic and Functional Neurosurgery (ESSFN) 2023, which took place from 27.09.-30.09.2023 in Stockholm/Sweden. The prize is endowed with €500.
June 2023
PD Dr. med. Ralf Weigel is now Associate Professor
Prof. Dr. med. Ralf Weigel was appointed adjunct professor by Prof. Dr. med. Michael Manns on 07.06.2023. Prof. Dr. med. Weigel has been working closely with the MHH since 2005 and is also a regular lecturer for student teaching.
14.06.2023
Neurological-Neurosurgical Wednesday Colloquium
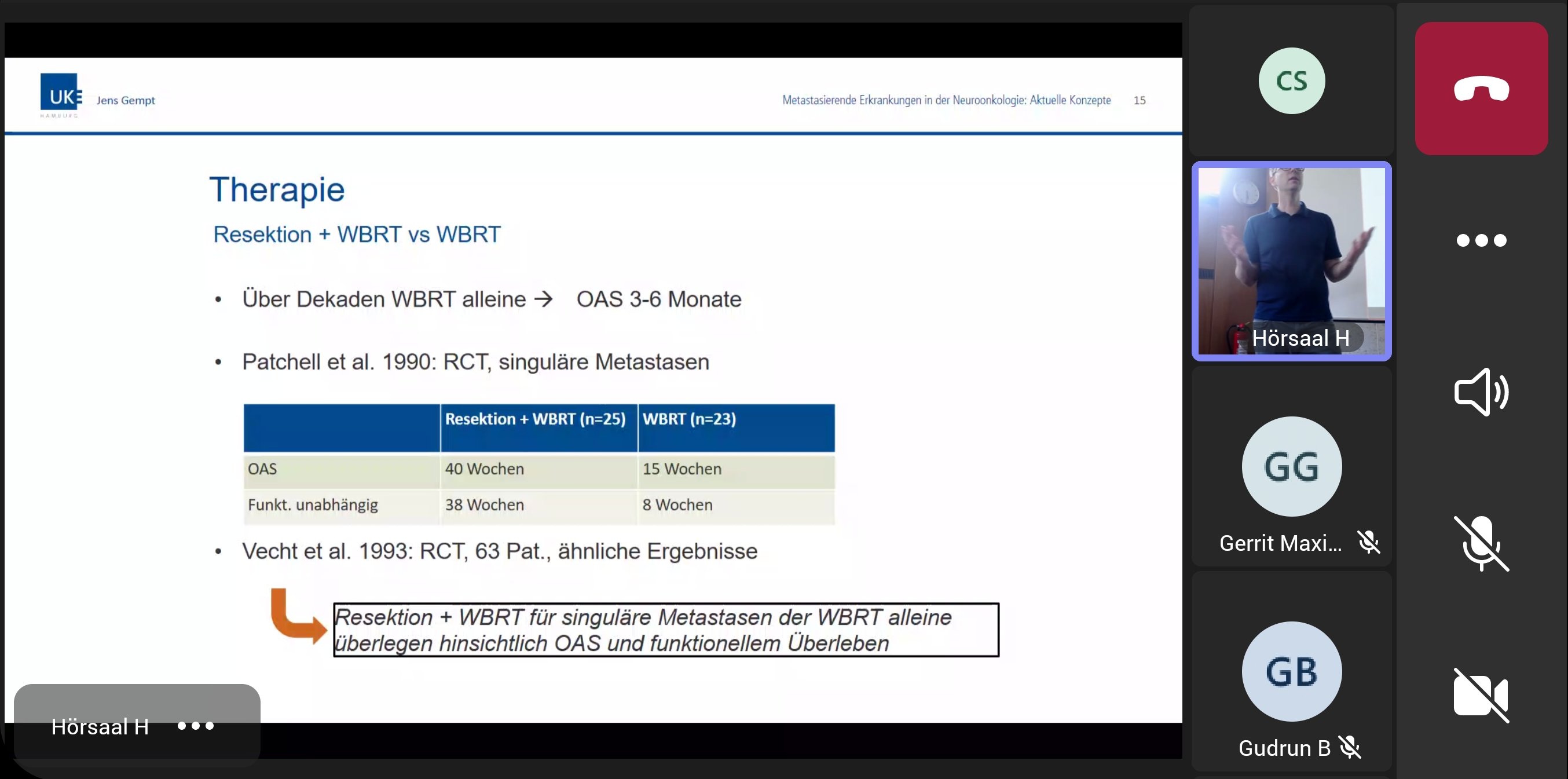
Prof. Dr. med. Jens Gempt, Director of the Clinical Department of Neurosurgery at the University Medical Center Hamburg Eppendorf, gave a lecture on "Metastatic Diseases in Neurooncology: Current Concepts".
The hybrid event was followed by 40 people in the lecture hall and 25 people online. As always, questions could be asked afterwards.
08.06.2023
Brain metastases: When cancer cells migrate from a primary tumor to the brain

Metastases are metastases of tumors. When a tumor first develops in an organ, it is referred to as a primary tumor. Cancer cells can then migrate from this original tumor via blood or lymph channels, spread to other organs and form a metastasis there, for example in the brain. On the occasion of World Brain Tumor Day on 8 June 2023, we talk to senior physician Dr. med. Majid Esmaeilzadeh from the Neurooncology Center at MHH about what brain metastases are and how they develop.
What is the difference between a brain tumor and a brain metastasis?
Most brain tumors are called gliomas, which originate from the brain tissue itself. Metastases are metastases of tumors that first developed in another organ and formed a so-called primary tumor there. Migrating tumor cells enter the brain via the bloodstream.
Do all cancers pose the same risk of developing metastases in the brain?
Statistically speaking, the risk is greatest for patients with lung cancer, breast cancer, renal cell carcinoma or malignant melanoma. In principle, however, almost any tumor can also spread to the brain. Therefore, brain metastases cannot be completely ruled out even in patients with other types of tumor.
Can anything be done to prevent it?
There are no specific measures that can be taken to prevent the development of metastases. It is always important that after a cancer diagnosis without metastases, the first cancer treatment, often surgery, chemotherapy or radiotherapy, is started as early as possible and that treatment is not discontinued. In general, a healthy lifestyle helps to reduce the risk of developing cancer.
How common are metastases in the brain?
In 20 to 30 percent of all cancer patients with systemic metastasis, metastases develop in the brain. The most common metastases are from bronchial carcinoma and breast carcinoma. Today, metastasis is the most common tumor in the brain.
The distribution of brain metastases:
- 40-60% bronchial carcinoma (lung cancer)
- 10-40% breast carcinoma (breast cancer)
- 10-15% malignant melanoma (black skin cancer)
- 10-20% no known primary tumor, 5% remain unknown
- 5% gastrointestinal carcinoma (digestive tract)
- 5% renal cell carcinoma
What can be signs of brain metastases?
Basically, the symptoms caused by brain metastases depend on their size and location. Many symptoms of brain metastases are relatively non-specific. The most common symptoms are headaches, neurological deficits such as paralysis and difficulty finding words or a so-called brain-organic psychosyndrome or an epileptic seizure. Dizziness, nausea and vomiting may also occur due to the accumulation of fluid around the metastasis.
How are brain metastases detected?
If a brain metastasis is suspected, various diagnostic procedures are available. Most patients undergo magnetic resonance imaging (MRI) or computer tomography (CT).
How are brain metastases treated?
Treatment depends on the location, number and size of the metastases. Several procedures are available for the treatment of brain metastases, which are discussed with the patient. These include surgical extirpation, i.e. the removal of the piece of tissue, radiosurgery, radiotherapy, chemotherapy and supportive measures such as psycho-oncology, speech therapy or physiotherapy.
...and what is the prognosis?
Brain metastases usually occur in the final stage of the metastatic process. The life expectancy of patients is therefore often limited. There are prognostic factors which, in addition to their significance for the survival prognosis, also play an important role in the treatment decision. These include the extent of metastasis outside the brain, the number of brain metastases, the time interval between the appearance of the primary tumor and the brain metastasis, the so-called Karnofsky Performance Score, an assessment tool for predicting the survival time of terminally ill patients, as well as age and histology.
10.05.2023
A perfect match for the treatment of brain tumors
Glioblastomas are malignant brain tumors with a poor prognosis, as they generally do not respond to conventional cancer therapies. One reason for this is that the tumor cells have developed mechanisms to evade the immune response. What's more, certain cells of the innate immune system, so-called tumor-associated macrophages (TAM), are influenced in such a way that they not only do not attack the tumor cells, but actually promote tumor growth.
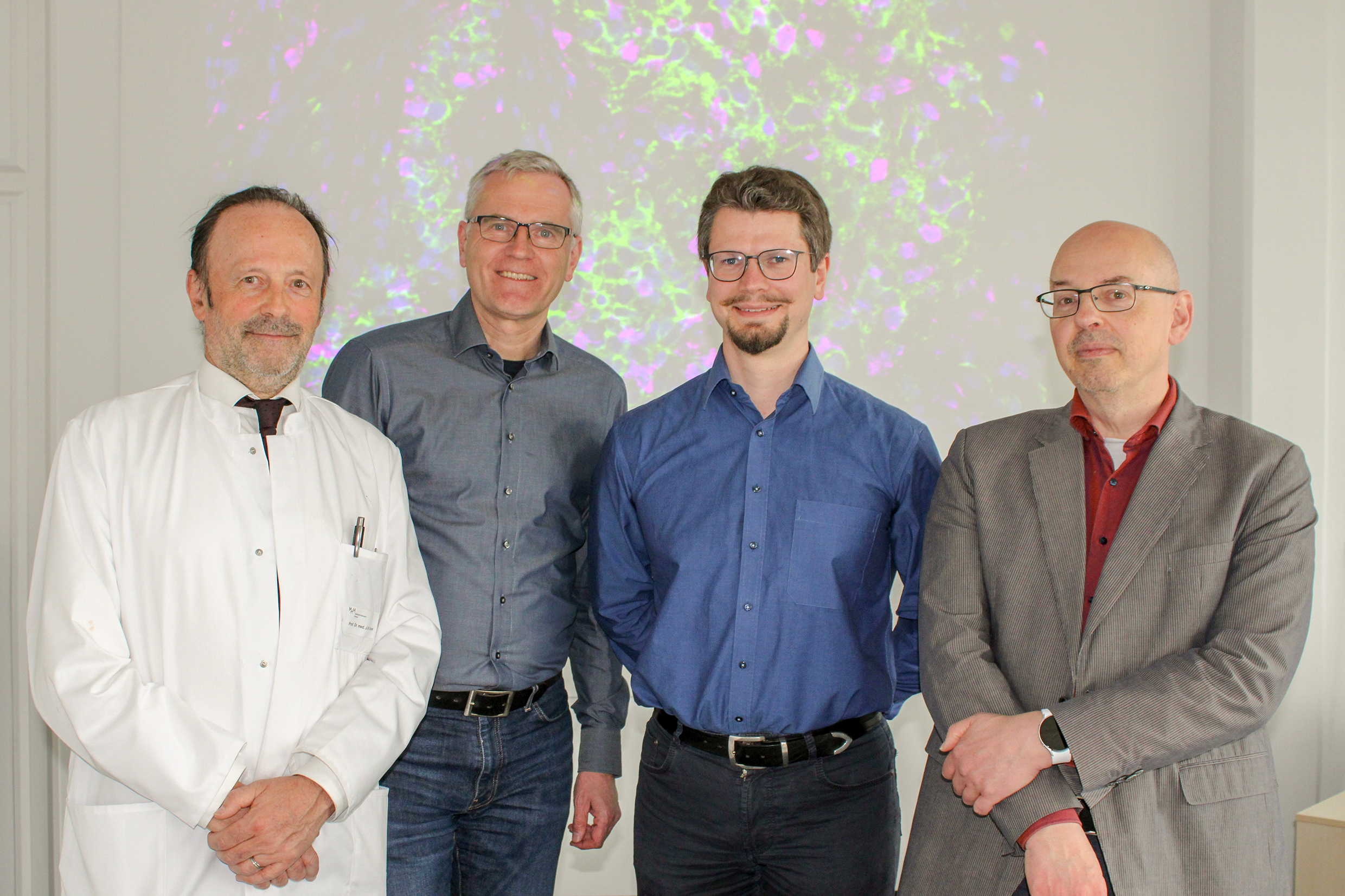
Researchers at the Institute of Clinical Biochemistry at Hannover Medical School (MHH), in collaboration with specialists from the Neurooncology Center led by Professor Hartmann from the Department of Neuropathology and Professor Krauss from the Department of Neurosurgery, as well as partners from the University Medical Center Göttingen (UMG), have now identified a new mechanism that improves survival in glioblastomas. The cross-site research under the umbrella of the Neurooncology Working Group of the Comprehensive Cancer Center Lower Saxony (CCC-N) was able to prove that patients with glioblastoma survive longer after resection of the primary tumor if the tumors produce a factor called polysialic acid and at the same time their TAM have an immune receptor called Siglec-16, which recognizes polysialic acid. The results were published in the renowned journal Clinical Cancer Research.
Tumor-inhibiting effect
"We observed a tumor-inhibiting effect in the trait combination of Siglec-16 and polysialic acid," says Prof. Dr. Herbert Hildebrandt, project leader in the DFG-funded research group 2953 "Sialic Acid as a Regulator in Development and Immunity" and research group leader at the Institute of Clinical Biochemistry at the MHH. "Through experiments on glioblastoma cells and macrophages in cell cultures, these changes could be directly attributed to the activation of Siglec-16 by polysialic acid".
"It is remarkable that, due to a naturally occurring gene mutation, only part of the population is able to produce Siglec-16, while polysialic acid was detected in over 80 percent of the glioblastomas examined," adds Dr. Hauke Thiesler from Prof. Hildebrandt's research group. "A simple genetic test in combination with other factors could enable a more precise individual prognosis." If it is also possible to mimic the activating properties of Siglec-16 with medication, this could help to improve glioblastoma therapy.
The original paper can be viewed via the following link.
You can find the press release here.
03.05.2023
Neurological-Neurosurgical Wednesday Colloquium
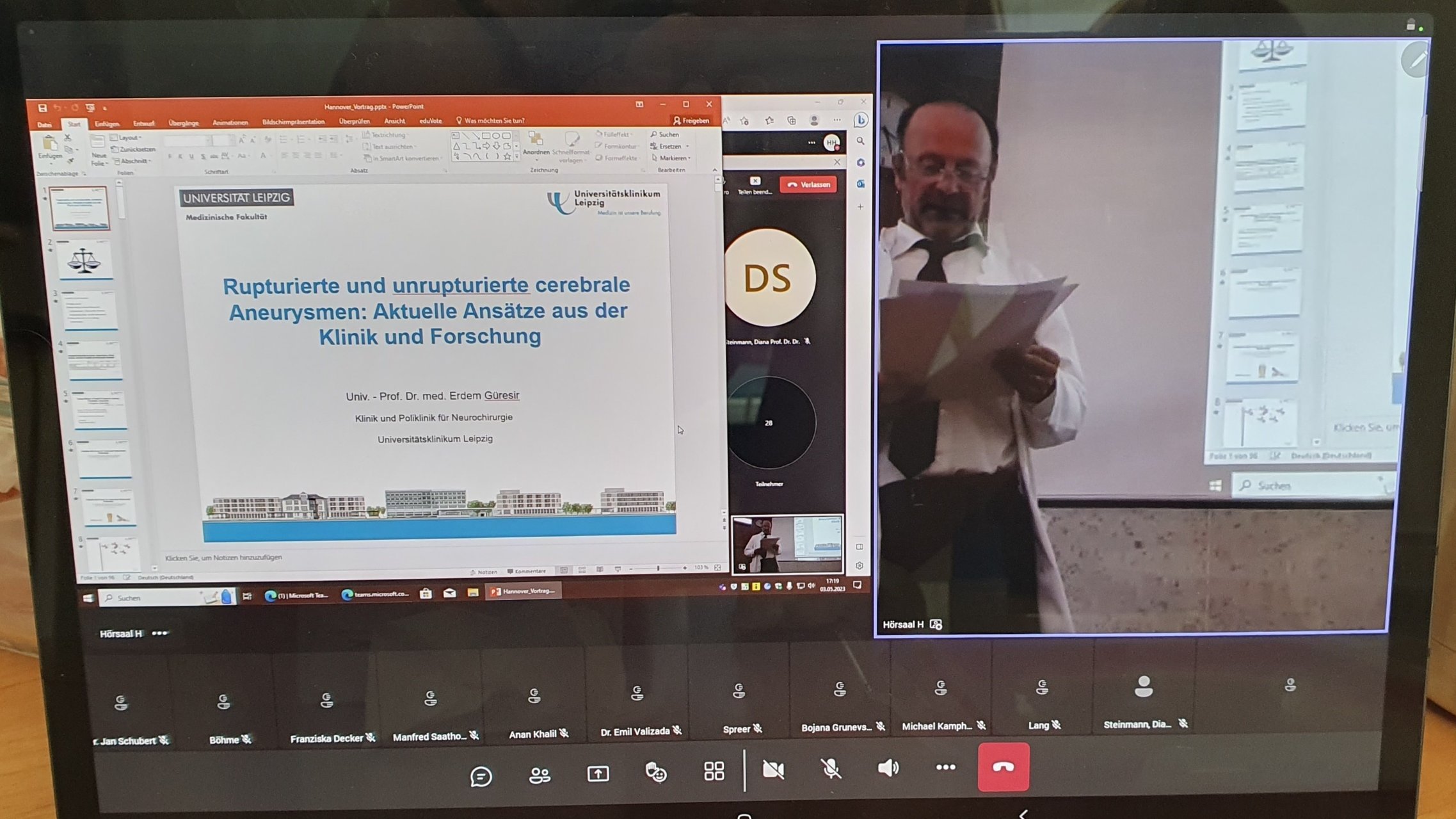
Prof. Dr. med. Erdem Güresir, Director of the Clinical Department of Neurosurgery at Leipzig University Hospital, gave a lecture on "Ruptured and unruptured cerebral aneurysms: Current approaches from Clinical Department & Research". This hybrid event was followed by 40 people in the lecture hall and 29 people online. As always, questions could be asked afterwards.
The picture shows an excerpt as an online participant. The lecture as well as the speaker, here Prof. Krauss in his moderation, can be seen.
19.04.2023
Dr. Esmaeilzadeh receives additional qualification in drug tumor therapy

Senior physician Dr. med. Majid Esmaeilzadeh has successfully completed the additional further training and now has the additional title "Drug-based tumor therapy".
Dr. med. Bettina Wiese and two other physicians at the Neurooncology Center now have this additional qualification.
April 2023
Revision of the Clinical Department of Neurosurgery website

The image shown is also available on the first page of the redesigned Clinical Department of Neurosurgery website and is intended to provide a direct and up-to-date reference. Ms. Claudia Schubert has redesigned the website.
- In a quick access on the first page of the NCH website, topics such as treatment spectrum, consultation hours, student internships & career, neuro-oncology center, neurosurgical research and contact options can be found quickly for the various interest groups.
- It is now possible to view videos of events and lectures by Prof. Krauss and his staff directly.
- All employees are now visible on the website with a photo.
- The online formats of the Neurological-Neurosurgical Wednesday Colloquium can be accessed directly in the News and Training section.
- It is also possible to access current topics, e.g. awards & appointments, publications, interviews and events, sorted by year.
March 2023
Podcast: The history of Stereotactic and Functional Neurosurgery and Serendipity
Prof. Krauss was interviewed together with Prof. Marwan Hariz and Prof. Christian Moll for a podcast by Prof. Andreas Horn (Boston).
Excerpt from Stimulating Brains:
"It was our great honor to talk with Joachim Krauss, Marwan Hariz, and Christian Moll about the history of Stereotactic and Functional Neurosurgery and the impact of serendipity in driving discovery. Our conversation was centered on two publications:
- Rzesnitzek L, Hariz M, Krauss JK. Psychosurgery in the History of Stereotactic Functional Neurosurgery. Stereotact Funct Neurosurg. 2020;98(4):241-247.
- Hariz M, Lees AJ, Blomstedt Y, Blomstedt P. Serendipity and Observations in Functional Neurosurgery: From James Parkinson's Stroke to Hamani's & Lozano's Flashbacks. Stereotact Funct Neurosurg. 2022;100(4):201-209.
In the first part of the episode, we reflect on the resonance of psychosurgery, talking about early pioneering work in this avenue. We delve into the fascinating history of Stereotactic Functional Neurosurgery, as outlined in Rzesnitzek et al.'s paper "Psychosurgery in the History of Stereotactic Functional Neurosurgery." We discuss the advances in technology and surgical techniques that have led to the current state of Stereotactic and Functional Neurosurgery, and the challenges and ethical considerations involved in this field.
In the second part of the episode, we explore the role of serendipity in driving discovery, inspired by Hariz et al.'s paper "Serendipity and Observations in Functional Neurosurgery: From James Parkinson's Stroke to Hamani's & Lozano's Flashbacks." We discuss the power of chance observations and unexpected findings in advancing our understanding of the brain and improving patient outcomes. We contrast the serendipitous approach to the more systematic methods of target discovery and debate the strengths and limitations of both approaches.
Overall, our conversation with Drs. Krauss, Hariz, and Moll shed light on the rich history and exciting future of Stereotactic and Functional Neurosurgery, and the fascinating interplay between serendipity and scientific discovery.
We hope you enjoy the conversation as much as we did and thank you for tuning in!"