Urogynecology / North German Pelvic Floor Center
Prof. Dr. med. Hermann Hertel

(Acting with competence
Sudden urge to urinate, incontinence or uterine prolapse - according to recent studies, one in three women suffers from at least one of these disorders. Many women believe that this condition is unavoidable and there is nothing they can do about it; the subject is often taboo.
Back in 2009, the Clinical Departments of Gynecology and Obstetrics, Neurology, Rehabilitation Medicine, Urology and Visceral Surgery at Hannover Medical School (MHH) founded the "North German Pelvic Floor Center". The aim is to treat women's pelvic floor problems comprehensively using an interdisciplinary approach.
Due to the significant demand for treatment options for pelvic floor problems and the far-reaching significance of urogynaecological clinical pictures for women's health, it is important to us to provide you with comprehensive care and special attention.
Contents
- Appointments / Registration - Where should I call?
- All about the pelvic floor
- The urogynecological consultation hour
- Genital prolapse / urinary incontinence
- Diagnostic and therapeutic spectrum
- Good to know
- Supporting offers
All about the pelvic floor
What is the pelvic floor?
A network of muscles and connective tissue that supports the organs; it plays a crucial role in bladder control, sexual function and posture.
Where is the pelvic floor located?
The pelvic floor lies like a hammock in the lower part of the pelvis and extends from the pubic bone (front) to the coccyx (back) and laterally to the ischial tuberosities.
How can I feel my pelvic floor?
You can feel your pelvic floor when you tighten the muscles that you would use to stop the flow of urine or hold back a bowel movement.
What are typical symptoms of a weak pelvic floor?
- Involuntary leakage of urine when sneezing, coughing or laughing
- Feeling of heaviness or pressure in the pelvis
- Pain during sexual intercourse
Do only older people have pelvic floor problems?
Problems with the pelvic floor can occur at any age, especially after pregnancy or during intense physical exertion.
The urogynecology consultation hour
The causes of pelvic floor problems are varied and can include constitutional, urological, gynecological, obstetric, proctological and age-related disorders or diseases of the pelvic floor. They require specialized diagnostics and therapy. The treatment methods include many options such as conservative therapy approaches by the Clinical Department for Rehabilitation Medicine through to minimally invasive, vaginal or proctological operations. Systematic diagnostics give affected women peace of mind. With the combination of interdisciplinary care and the application of the latest therapy options, even complex problems can be overcome. Supporting services round off our range of treatments.
Urogynecology includes the treatment of various forms of incontinence and prolapse of the internal genitalia, such as
Genital prolapse or descensus uteri et vaginae is a prolapse of the internal female genital organs in the small pelvis. Due to their close connection with the neighboring bladder and rectum, these organs are almost always affected. The lowering of the uterus and vagina up to the hymenal seam is referred to as descensus and lowering beyond this as prolapse.
In the last 10 years, the ICD diagnosis of genital prolapse has risen steadily in German hospitals. Descensus operations are therefore one of the most frequently performed gynecological operations.
The pelvic floor forms a stable, lower closure in the small pelvis. The pelvic organs are held in their physiological position by connective tissue and muscular connections with the pelvic bones, without restricting their mobility.
In general, prolapse damage is the result of an imbalance between the load and resilience of the pelvic floor. In most cases, it is a multifactorial process that progresses over time. The most important risk factors are Pregnancy due to hormonal changes in the pelvic floor connective tissue, births that cause pelvic floor weakness, trauma with muscle/nerve injuries due to excessive stretching/compression (e.g. forceps delivery), age due to a reduction in oestrogen levels with atrophy of the tissue and connective tissue weakness as a genetic predisposition. Everyday factors are obesity, chronic coughing in smokers or bronchitis, constipation, heavy physical work. Common symptoms of prolapse are Urination disorders, a feeling of pressure or heaviness in the lower abdomen, pulling lower abdominal and back pain, a bulging sensation in the vagina, constipation, urinary incontinence, inflammation. This wide range of symptoms can have a considerable impact on those affected, both physically and psychosocially.
Another main area of urogynaecology is urinary incontinence. Unfortunately, this issue is all too often concealed by those affected. Minor problems are concealed, more severe forms are unfortunately tabooed out of shame.
This leads more and more to restrictions in everyday life, giving up physical activity and giving up hobbies. However, after appropriate diagnostics, it is possible to significantly alleviate the symptoms and thus improve quality of life. There are basically two types of incontinence, which are the most common.
In the case of "overactive bladder" (synonym: irritable bladder, urge bladder, urinary incontinence, OAB; overactive bladder), patients experience a strong urge to urinate with frequent trips to the toilet at night and during the day with only small amounts of urine or they lose urine unintentionally and unstoppably after short, strong urges. The cause is an overactive bladder muscle that causes urge and may contract independently of the patient's will and empty the urine from the bladder. The quality of life is considerably impaired, and a reduction in the amount of urine drunk further exacerbates the symptoms.
Stress incontinence is the second most common type of incontinence. In this case, urine leakage occurs during physical exertion such as coughing, laughing, sneezing and lifting. The cause is a weak bladder closure muscle around the urethra. This can be caused by childbirth, weak connective tissue, obesity, chronic lung diseases and hormone deficiency.
We offer you a wide range of innovative and proven examination and treatment procedures for genital prolapse and/or urinary incontinence
Whether incontinence or prolapse complaints, there are often transitions and similarities in the complaints and diagnoses, so that our diagnostic spectrum initially serves to record the entire urogynaecological status.
The diagnostic spectrum of urogynaecology for prolapse and incontinence complaints includes
- Incontinence questionnaire,
- micturition protocol,
- Gynecological status,
- pelvic floor assessment,
- Urogenital and perineal sonography,
- urethrocystoscopy,
- Urodynamics with cystotonometry,
- urethral pressure profile and uroflow
After a detailed consultation, examination and diagnosis, we offer a wide range of conservative and surgical treatments.
The therapeutic spectrum for gential lowering (descensus treatment):
Initially conservative therapy for incipient descensus:
- Biofeedback,
- electrostimulation,
- pelvic floor training in close cooperation with the Clinical Department for Rehabilitation Medicine,
- vaginal reconstructions for cystocele / bladder prolapse (central defect) and/or rectocele / posterior prolapse,
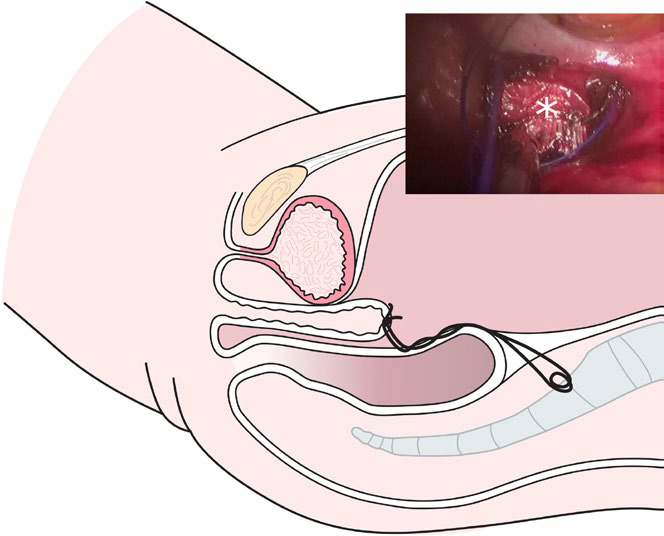
- vaginal sacrocolporectopexy (vaginal fixation for uterine and/or vaginal prolapse) as a gentle surgical method, also under spinal anesthesia (Fig. 2),
- vaginal uterosacropexy (preservation of the uterus in cases of uterine prolapse) and
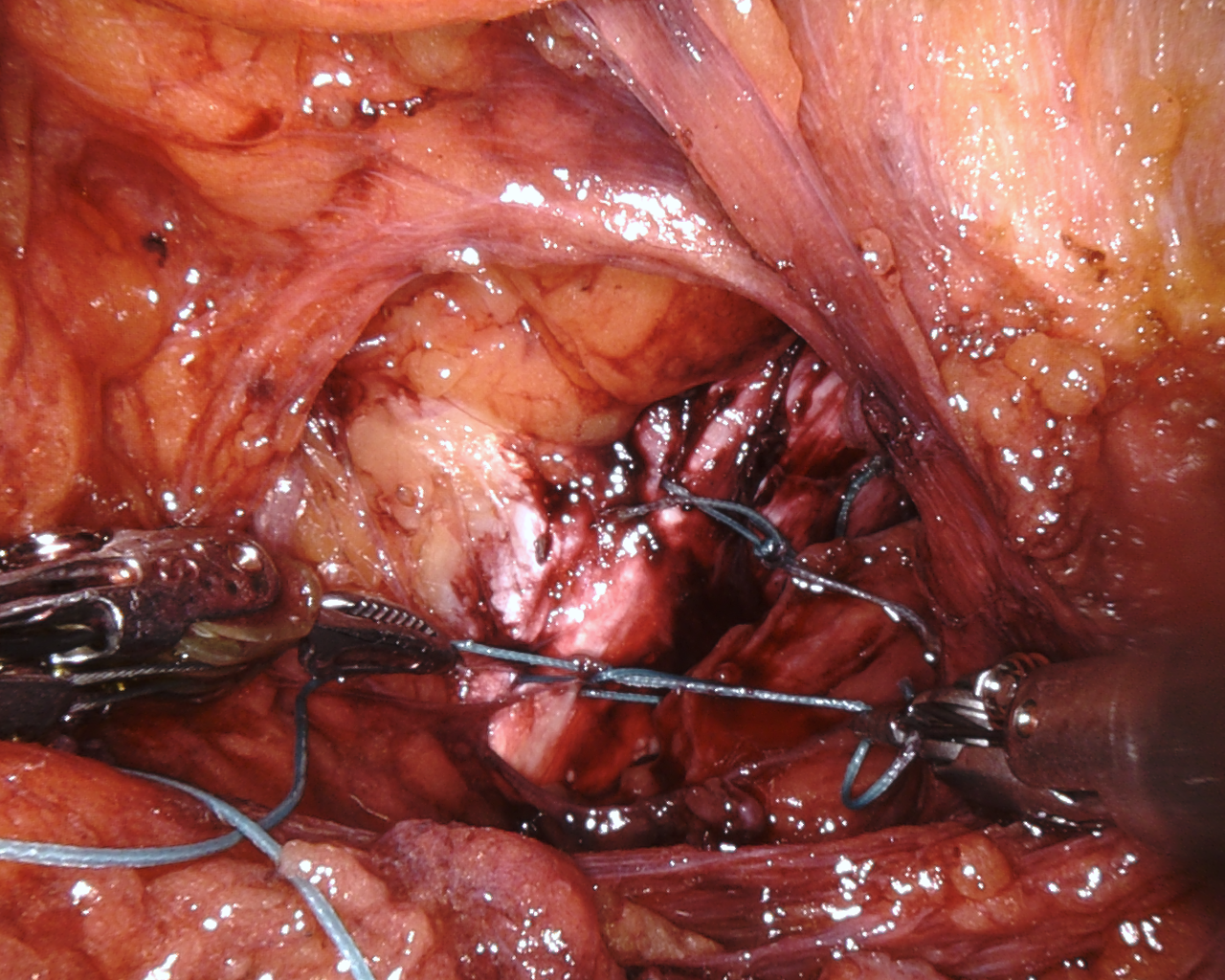
- laparoscopic lateral repair without touching the vagina from the vaginal side (minimally invasive vaginal fixation for lateral vaginal prolapse / cystocele / bladder prolapse / lateral defect (Fig. 3)), here also with the help of the da Vinci surgical robot system.
The vaginal end (or the uterus) is fixed in the direction of the sacrum with a stable suture. A laparoscopy or abdominal incision is not necessary and nets are not used.
The therapeutic spectrum for urinary incontinence:
Range of intensive conservative therapies for incipient urinary incontinence:
- Biofeedback,
- electrostimulation,
- pelvic floor training in cooperation with the Clinical Department for Rehabilitation Medicine,
- Tension-free polypropylene tapes (TVT tape, retropubic), also under spinal anesthesia,
- Colposuspension according to BURCH (laparoscopic, open surgery), especially in the recurrence situation or in younger patients, here with the help of the da Vinci surgical robot system (Fig. 3/4).
- Alternatively, hysterosacropexy, i.e. minimally invasive injection around the urethra with a special plastic depot, can be considered. This is an option if anesthesia is not an option, a more extensive procedure is to be avoided or in a recurrence situation with multiple previous therapies.
Alongside physiotherapy, medication is the leading treatment methodfor urge incontinence.
Organ preservation and mesh-free treatment are very important to us, especially for young women who wish to have children.