Obstetrics
Univ.-Prof. Dr. med. Constantin von Kaisenberg

Anyone expecting a baby is at the beginning of a wonderful but also great challenge. Many questions accompany the young parents: How should our baby be born? Do we need special support? What options are available to help me cope with the pain? And many more questions ...
We are at your side with help and advice from the beginning of your pregnancy to your discharge, so that you can enjoy this time carefree. You are the center of attention and we are there for you.
Table of contents
- Appointments | Registration - Where should I call?
- Registration for birth (incl. form download)
- What happens in the consultation hours of the antenatal clinic?
- Information evenings for parents-to-be
- More about obstetrics and the delivery room
- Midwives for pre- and postnatal care
- Supporting offers
Birth registration
Desired/recommended from the 20th week of pregnancy

Download form:
- Registration for birth (pdf file)
- Contract for elective medical services
- Elective service agreements for non-medical elective services
Please fill out the registration form (including the attachments if required) as completely as possible and send it with your signature
by post to:
Hannover Medical School
Clinical Department of Gynaecology and Obstetrics
- OE 3812 / Delivery Room -
Carl-Neuberg-Str. 1
30625 Hannover
No written confirmation will be sent
What happens in the consultation hours of the antenatal clinic?

At the beginning of each examination, an ultrasound scan is carried out to assess the child's position, weight and care situation. The obstetric history is then taken in a discussion with you. The various delivery options are then presented - in particular, the current study situation is discussed. The risks and complications of a vaginal delivery and a caesarean section will be explained. The particularities of the delivery will be discussed together. The birth process itself is presented and explained with the help of a birth model.
After a detailed explanation and assessment of the findings, further follow-up checks will be arranged until you have decided on a mode of birth based on the clinical parameters and information about the process and special features of the individual options. In this way, you become the experts yourself and can decide on the basis of as much information as possible.

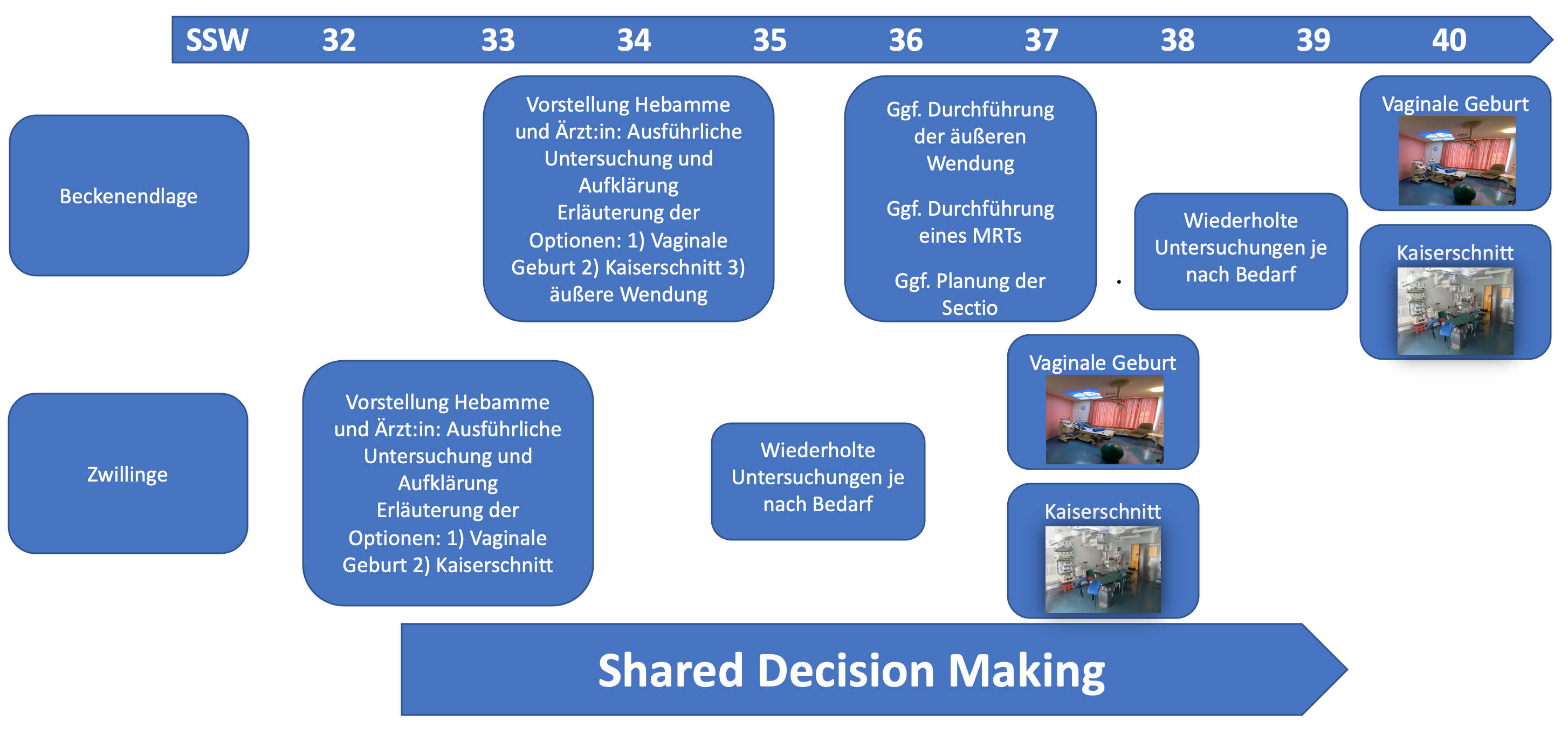
Is your baby in a breech presentation or are you expecting multiples? Then you've come to the right place!
Around 3% of all children are in a breech position at term, and twin pregnancies occur in around 1.4% of all cases. These obstetric cases are therefore rare, but at the same time there is a need for individual advice and care.
In Germany, more and more children are being born by caesarean section. In many cases, this type of birth is not absolutely necessary from a medical point of view. If a pregnant woman is expecting twins or the unborn child is in a breech position, this does not automatically mean that she can only give birth by caesarean section.
Our interdisciplinary consultation for breech presentation and twins consists of an experienced midwife and a senior physician and takes place every two weeks.
We support expectant mothers during the last weeks of pregnancy. We want to make you an expert in your pregnancy so that you can make a self-determined and evidence-based decision on the mode of birth.
Due to the controversial studies on the "optimal" mode of birth, there is a great need for detailed advice and support. It is also essential to consider your own wishes, needs and experiences.
Information evenings for expectant parents
Again in presence - on site and as a live video chat

The focus is on all topics relating to pregnancy, birth and the postpartum period.
Our obstetrics team offers an information evening twice a month so that parents-to-be can find out about our obstetrics department and feel well prepared.
Afterwards, there is the opportunity to familiarize yourself with the maternity ward and the delivery rooms and to ask personal questions.
The events take place on two Mondays a month. Alternating between face-to-face events and online events every two weeks at 6:30 pm.
Our themed parents' evenings also offer you special information on preparing for the birth and being a parent.
- 15.12.25
- 05.01.26
- 02.02.26
- 02.03.26
- 30.03.26
- 27.04.26
- 01.06.26
- 29.06.26
- 27.07.26
- 24.08.26
- 21.09.26
- 19.10.26
- 16.11.26
- 14.12.26
Interested parties can obtain the access data for the live transmission via the Microsoft Teams program by sending an informal e-mail to geburtshilfe.infoabend@mh-hannover.de.
The technical requirements are a computer with an (integrated) camera, microphone and speakers or headphones. Access is also possible with a tablet or smartphone.
- 19.01.26
- 16.02.26
- 16.03.26
- 13.04.26
- 11.05.26
- 15.06.26
- 13.07.26
- 10.08.26
- 07.09.26
- 05.10.26
- 02.11.26
- 30.11.26
More about obstetrics and delivery room
EVERYTHING UNDER ONE ROOF!
Safety, for mother and child, is always our top priority. As a Level 1 Perinatal Centre, we are prepared for any situation at any time, around the clock, 365 days a year. We are an experienced, dynamic and international team consisting of midwives, gynecologists, anesthesiologists and pediatricians. All disciplines are on duty for you on site, work very closely together and are in constant contact with each other.
We are a university hospital and therefore a super-maximum care facility. With this safety net and our highly competent obstetric team, we support you throughout the entire birth process and look forward to caring for you in a pleasant atmosphere - both during an uncomplicated pregnancy and in the event of problems.
The presence of your partner or a companion during delivery and also during a caesarean section, early skin-to-skin contact (bonding) even after a caesarean section can help you and your baby get off to a good start in life together.
Free choice of birth position, water birth, outpatient delivery, spontaneous birth in a breech presentation, external turning in a breech or transverse presentation in a cephalic position are all possible.
We will be happy to advise you on all methods of pain relief during childbirth.
Room facilities
Every year, around 2500 children are born in our five bright and modern, but also comfortably equipped delivery rooms. With a view of the park and two monitoring rooms, we enable you to organize the birth according to your wishes and needs. All rooms are equipped with comfortable, electrically operated multifunctional delivery beds with integrated birthing stools that allow for any birthing position. The women giving birth can move freely around the birthing room using wireless heartbeat monitoring. This allows them to assume different positions at any time. We also offer a birthing tub - birthing stool - birthing mats - wall bars - mobile swinging cloth - hanging rope - Pezzi balls, aroma lamp and stereo system, two bathrooms with relaxation bathtub, changing lighting system and music, as well as relaxation chairs for the father. We motivate the women giving birth to adopt alternative birthing positions. Whether it's a quadrupedal position, stool birth or delivery in the warm water of the birthing tub - we cater to every wish, as far as medically justifiable.
In order to be prepared for all eventualities, a modern operating room for caesarean sections and two neonatal resuscitation wards are integrated into the delivery room area. By means of an emergency caesarean section alarm, we are able to perform an emergency caesarean section within a very short time. When the alarm is triggered, obstetricians, anesthetists, operating room staff and pediatricians are automatically informed.
Two spacious, bright rooms are available so that you can rest and gather strength for the upcoming delivery beforehand or for more intensive observation.

All women who require inpatient clarification, monitoring or treatment during their pregnancy are in good hands on our prenatal ward, ward 84.
We provide a widerange of care: we perform cervical closures to prevent miscarriage or premature birth, treat women in premature labor to prevent premature birth, monitor and treat children while they are still in the uterus, treat pregnancy-related illnesses such as diabetes or pre-eclampsia and care for all patients who have a higher risk for the current pregnancy due to a concomitant illness.
Close cooperation with other specialist departments involved enables optimal treatment. Whenever necessary, experts from nephrology, surgery, neurology, cardiology and many other specialist departments come together to determine the right treatment strategy together with the patient.
The simultaneous nursing care provided by nurses and midwives on the ward ensures that the most diverse concerns always find an optimal contact person.
Medical care is provided in close cooperation with prenatal medicine and the delivery room, so that all important clarifications, in particular ultrasound examinations, can always be carried out directly and quickly and further planning of the pregnancy can be initiated immediately.
All women who have been admitted for childbirth or have already given birth are accommodatedon the mother and child ward. We follow a holistic, family-friendly care concept, whereby we see the entire family as a unit.
Our nursing team consists of full-time and part-time registered nurses, some of whom have additional qualifications as IBCLC breastfeeding and lactation consultants. Midwives, nurses and pediatric nurses work together in an integrative manner. Participation in internal and external training courses is an integral part of our Human Resources. New colleagues are introduced to their tasks in accordance with an induction guideline developed by our ward, which guarantees our patients a high standard of safety and care.
Children who require additional monitoring, such as suitable premature babies, can remain on the ward's own child monitoring ward, where six beds are available. This means that the children always remain close to their mother, even if they need additional care.
A pediatrician is explicitly available every day to look after the monitoring ward and carry out regular examinations of the newborns.
The rooms are set up to accommodate a maximum of two patients per room. They can also be used as single or family rooms.
- Did you know?
Physiotherapy in the puerperium
Our care and support on the mother and child ward 82
We, the obstetrics team at Hannover Medical School (MHH), provide parents with advice and support from the beginning of their pregnancy to discharge and beyond. The central aim of our holistic concept is to prepare you and your family members for the birth and life with the newborn. We offer further guidance and support beyond the hospital stay. Our comprehensive parent education courses provide answers to questions during the exciting time of pregnancy and birth, so that you can prepare well for the new life with your baby. We are also there for you after the birth. From our comprehensive range of courses, you can choose the modules you want as a foundation for becoming and being a parent.
We recommend breastfeeding right from the start. Our IBCLC breastfeeding and lactation consultants and staff trained in theory and practice are on hand to provide mothers with helpful tips and information.
Bonding
We enable parents to have undisturbed, extensive skin-to-skin contact with their child, as far as medically justifiable, for at least 1 hour after birth or until the baby is breastfed for the first time. This primary bonding helps the child to develop and strengthen its innate abilities to explore its environment and interact with it, allowing the baby to adapt well to its new environment. Breathing, circulation and body temperature stabilize. For full-term babies, we recommend continuing this skin-to-skin contact after birth and during the time when the mother/father are awake.
Even after a caesarean section, the baby can have skin-to-skin contact as soon as possible. If your child is born prematurely, it can usually cuddle with you in direct skin-to-skin contact after it has been examined and cared for by the pediatricians and before it has to be transferred to the children's hospital. This is even possible if breathing assistance is required. This allows you to build up an intensive relationship with your baby straight away.
Importance, short and long-term effects of skin-to-skin contact with your baby
- Continued safety and security for the baby, 9 months of not being alone.
- The release of the breastfeeding hormones prolactin and oxyocin is encouraged. This leads to you and your baby relaxing together. You can react very quickly to your baby's signals.
- The baby finds its way to the breast through skin-to-skin contact, making it easier to start breastfeeding. Your baby intuitively knows how to find and grasp the breast.
- Promoting the mother/parent child relationship through skin-to-skin contact regardless of how you feed your baby.
Many studies confirm this:
- The baby cries less.
- Milk production is stimulated.
- Breastfeeding works better.
- The baby gains weight better.
- You become more confident with your baby.
24-hour rooming-in
Healthy, vital premature and newborn babies and their mothers are not separated from each other. Mother and child are cared for by a nursing specialist. They receive the help and support they want and need around the clock to care for their child. The competence in dealing with the baby lies with the parents. The early intimate contact and the closeness of being together help, for example, to understand the baby's signals more quickly and to react to them.
Breastfeeding - nourishment for body and soul
Breast milk is the most natural food for the newborn and breastfeeding strengthens the bond between mother and child. We encourage women to breastfeed and are happy to help with the first and correct latch-on or the collection of breast milk.
Breastfeeding according to the needs of the child and mother is ideal. It may be necessary to wake the baby to relieve the mother's breast or so that the baby can be adequately nourished.
In healthy, mature newborns, there is no need for additional feeds when breastfeeding on demand. We will inform you if there is a medical indication for this. If supplementary feeding is necessary, we recommend using alternative feeding methods - we do not give breastfed children teats or pacifiers in order to disrupt the start of the breastfeeding process as little as possible.
If physical separation is necessary, e.g. from a premature or sick child, we instruct the mother on how to initiate and maintain milk production and feed the baby with expressed breast milk. After all, breast milk is particularly important for sick or premature babies.
- Breast milk makes the difference - Find out about the importance of breastfeeding, colostrum - the power milk of the first few days, nipple care and more...
- And, did you know? Simply the best. Breast milk is the best choice for diabetes
Support in the home/family environment
Back at home, we offer mothers support through our breastfeeding hotline and breastfeeding groups in addition to the topic-specific courses at the Parents' School. For individual consultations, the Parents' School of the MHH Women's Clinic offers a breastfeeding outpatient clinic.
Parents who have lost a child are referred to as orphaned parents.
Farewells and separations, dying and death are aspects of our lives. For parents who have lost a child before, during or shortly after birth, we offer a special care concept at the Obstetrics Department of Hannover Medical School (MHH).
Please contact us at
Tel.: +49 (0)511 532 6865 Halina Huppertz, Senior Midwife
Psychological support is available at any time via the Gynecological Psychosomatics Department.
Phone: +49 (0)511 532 9550
This might interest you
As a mother-to-be expecting your baby, you will have given a lot of thought to the forthcoming birth and you will have many questions. You will be particularly concerned with the question of how much pain such a birth means and whether there is a way to alleviate the pain. The decision for or against a pain-free birth is a very individual one, as every woman experiences the birth of her child differently and labor pains are experienced with varying degrees of intensity.
Modern anesthesia offers effective and safe procedures to alleviate labor pain. As a result, unlike in past centuries, no expectant mother has to endure untreated pain. Peridural analgesia via a pain catheter (epidural) is a particularly proven method for a pain-free birth. But:
- How does it work?
- Who does it?
- Is it dangerous for my baby or for me?
- Are there any side effects?
- Does the anesthetic last long enough?
- What alternatives are there?
We would like to discuss these and other questions with you during an informative consultation so that you are well prepared for a safe and pain-free birth that is individually planned for you!
Please note that we can only perform epidural analgesia on you if we have been able to talk to you in advance of your planned birth. A consultation on the actual date of birth or even during the birth is only possible in exceptional cases!
Please register without prior appointment Tuesday to Friday from 11:00 am to 1:00 pm at the patient registration desk of the Women's Clinic (Building K11, Level S0) and then come to the open anesthesia consultation forpre-medication here on the 2nd floor in front of ward 83.
Please report/register at the patient admission desk without pre-registration and then come to the anesthesia consultation here on the 2nd floor in front of ward 83 for premedication. Our staff will be happy to welcome you.
Spontaneous breech births on the increase. Approximately 3-5% of all children are in breech presentation in the third trimester of pregnancy.
If the child has not turned into the cephalic position by 35 weeks' gestation, we offer an appointment in our antenatal clinic. We often suggest an outpatient external turning in the cephalic position in the delivery room.
The number of vaginal deliveries from a breech presentation has recently increased significantly at MMH. Experienced obstetricians accompany the pregnant women during a spontaneous BEL delivery. Spontaneous BEL deliveries are currently performed in the transverse bed, usually with manual assistance according to Bracht or arm release according to Bickenbach and development using the Veit-Smellie maneuver.
Annual multi-professional team training takes place in the PROMPT courses (organized by Prof. von Kaisenberg and team) and thus ensures a high obstetric standard.
Since 2020, the MHH has been the first FIGO-trained pelvic presentation birth center in Germany.

Another concept is the delivery of the child from the pelvic presentation from the quadrupedal position. This concept was introduced by Prof. Dr. Dr. h.c.. F. Louwen. His approach has since led to the University Clinical Department in Frankfurt becoming a FIGO-certified training center for breech deliveries worldwide.
After the umbilical cord has pulsed out, the vessels of the placenta and the remaining part of the umbilical cord still contain blood that is no longer needed by the newborn and its mother. This umbilical cord blood is routinely disposed of and incinerated like all other biological waste products in accordance with the applicable national regulations.
At the MHH, however, you can decide to donate the umbilical cord blood for research in order to further improve medical care for pregnant women and their children in the future.
Research projects to which you can currently donate umbilical cord blood:
Prepare for your birth:
With our birth preparation course, you'll be well prepared for the birth!
A space for all your questions:
With valuable knowledge, techniques and space for all your questions - together we ensure safety and self-confidence.
What happens when I arrive in the delivery room?
You will be greeted, asked about your well-being and have to answer a few questions.
What will I be asked for when I arrive at the hospital?
- Maternity passport
- How many weeks pregnant is it?
- Which week?
- When did the bladder rupture?
- Strength of the contractions
- Abnormalities
- Bleeding
What if I'm already in labor?
We will measure your blood pressure and take a CTG to assess your baby's heartbeat. We may also be able to see how regular your contractions are.
Will I also be examined?
Depending on your week of pregnancy, you may have a vaginal examination and an ultrasound scan.
Can I then stay in the delivery room?
We will then decide whether you will be admitted as an inpatient or whether you can go home again.
First of all: stay relaxed!
Because contractions are the most natural way to start labor.
There are different types of contractions:
- In the beginning, contractions usually come at longer, irregular intervals and do not last long.
- Over time, contractions become longer and more regular.
To give you an idea of when you can start:
- 1st child: 2 hours of constant contractions lasting 3-5 minutes
- from the 2nd child: 1 hour of constant contractions lasting 5-7 minutes
- the length of the contractions should be one minute
- this is for orientation and is different for every woman giving birth
Ideas of what you can do at home:
- Relaxing bath
- Warm shower
- sleep
- Listen to music
- Go for a walk
Good to know:
Every woman giving birth can stay at home for as long as she feels comfortable.
In general:
If you are unsure, you can also contact us by telephone at any time.
First of all:
Stay relaxed!
Self-examination:
- Are you 37+0 weeks pregnant?
- Is the amniotic fluid bright clear and pink?
- Is your baby moving normally?
- Is the head firmly in the pelvis?
Yes? Then you are welcome to take a little more time before you make your way to us!
You should make your way to us as soon as possible:
- prematurity
- green amniotic fluid
- Streptococcus B positive
- breech presentation
- transverse position
- multiple birth
- Head not firmly in the pelvis
If one or more of these criteria apply to you, you will be informed in advance and we will discuss what you should do.
Good to know:
Due to the increased risk of infection from ascending germs, we usually start antibiotics 12 hours after rupture of the membranes.
If you are unsure, you can contact us at any time!
There are different names for the surgical method of bringing a child into the world:
- Cesarean section
- caesarean section
- Abdominal delivery
- Abdominal delivery
- C-section
- Ceasarean section
There are four types of caesarean section:
- Primary caesarean section:
- is performed on a scheduled date
- neither a rupture of the membranes nor contractions affecting the cervix are a prerequisite
- is independent of the natural onset of labor
- Secondary caesarean section:
- unplanned - is performed in the event of labor arrest
- Birth has already begun, i.e. both rupture of membranes and contractions are present
- can take place at rest, there is enough time for spinal anesthesia/PDA
- urgent cesarean section:
- Cesarean section should take place within 30 minutes of the indication
- Can be primary or secondary
- there is usually enough time for necessary explanations, etc.
- Spinal anaesthesia is possible
- Emergency caesarean section:
- Should be performed if the life of the mother and/or child is at risk
- Caesarean section within 10 minutes of the indication
- Always performed under general anesthesia
Good to know:
In consultation with the medical staff, you can still give birth vaginally after a caesarean section.
Interested?
Would you like to become a midwife and help parents with the birth of their child as well as look after families before and after the birth?
Then apply to Hannover Medical School!
What makes our study programmes special?
Our study programmes offer practical learning and teaching from interdisciplinary lecturers at a medical university.
Course content at a glance
-
Everything to do with pregnancy, birth and postpartum
-
Knowledge of anatomy, physiology and pathology
-
Support for expectant parents and their emotional needs
Duration:
7 semesters (3.5 years)
Degree:
Bachelor of Science in Midwifery Science - Bachelor
Career opportunities
-
Freelance or employed midwife
-
Obstetrics in hospitals, birth centers or at home
-
Outpatient care and services for women and families
-
Academic career or further training in specialized areas
Application tips
-
University entrance qualification
-
Proof of a 4-week pre-study internship
-
Medical health certificate
-
Proof of measles vaccinations
Good to know:
The application deadline for the respective winter semester is always from June 1 to July 15 of each year.










