The Breast Center of the MHH
Dr. med. Elna Kühnle

The Breast Center at Hannover Medical School (MHH) is the central institution for questions relating to the diagnosis and treatment of breast diseases.
Breast cancer is of particular importance here. We offer women and men with breast cancer a holistic care concept whose high level of professional competence has been tested and certified by independent experts in accordance with the requirements of the German Cancer Society, the German Society for Senology and DIN EN ISO 9001.
Contents
- Dates | Registration
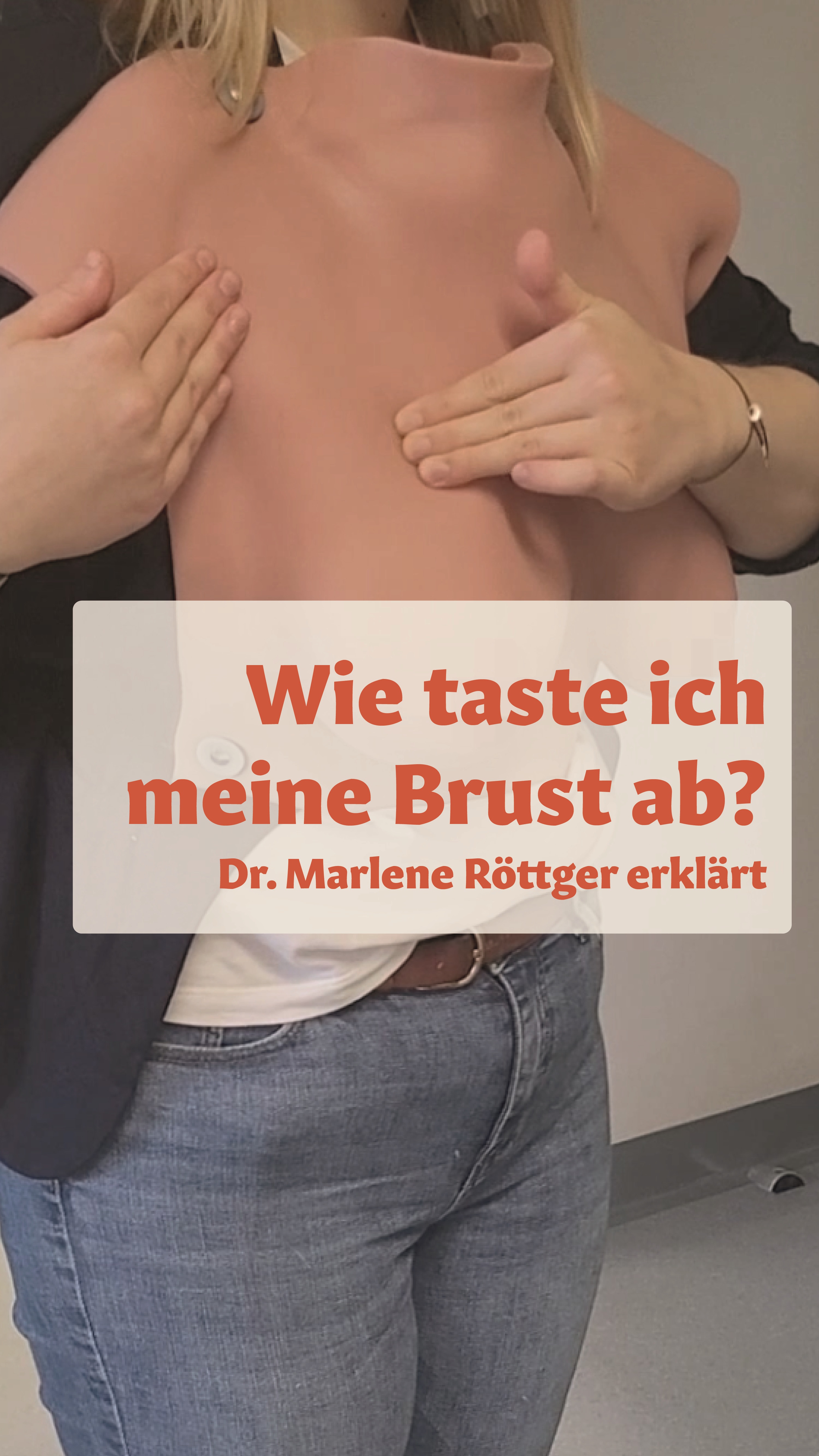
- Video: How to scan my breast
- Our area of responsibility
- Our services
- Good to know
- Supporting offers
Our area of responsibility
At our Breast Center,we care for patients who have been diagnosed with breast cancer for the first time as well as those who have suffered a recurrence or have metastatic disease. We see it as our task as a university hospital to offer them the best possible surgical and drug therapy at all times, which corresponds to the latest scientific findings and to create an individualized treatment concept for each patient.
We see it as our task as a university hospital to offer our patients the best possible surgical and drug therapy at all times, which corresponds to the latest scientific findings and to create an individualized treatment concept for each patient.
The interdisciplinary structure of the Hannover Medical School (MHH) - everything under one roof - and the close cooperation enable our patients to be referred directly to colleagues in radiotherapy, thoracic surgery, plastic surgery or internal medicine.

Our holistic approach also includes supporting measures. In addition to the connection to gynecological psychosomatics and psycho-oncology, we also provide nutritional medical support and traditional Chinese medicine (TCM) therapy options if required.
Above all, we appeal to your self-care, self-examination and early detection.
Services
Early detection of breast cancer can often mean gentler treatment and improve the chances of recovery. In many cases, small tumors detected at an early stage can be treated with breast-conserving surgery. Based on the histological examination of the tissue sample (punch biopsy) by the pathologists, a targeted and individualized therapy can already be determined for most patients.
Mammography screening
All women between the ages of 50 and 69 receive an invitation to a free mammogram every two years as part of cancer screening. Mammography screening in Hanover is organized by the Central Office of the Association of Statutory Health Insurance Physicians of Lower Saxony.
Familial breast and ovarian cancer
The MHH Breast Center is part of the German Consortium for Familial Breast and Ovarian Cancer in Germany. In 5 - 10% of all breast cancer cases, the disease is hereditary. A very young age of onset, the occurrence of breast and ovarian cancer in several members of the maternal and paternal line or the occurrence of breast cancer on both sides can be indications of a genetic cause.
If there is a certain risk constellation, genetic testing can be carried out using a blood sample in the Department of Human Genetics at the MHH.
- Mammography
Mammography is an indispensable component of breast diagnostics. This X-ray examination can be used to detect lumps in the breast as well as conspicuous calcifications in the breast. In special cases, for example when patients have very dense glandular tissue, we can take and evaluate additional tomographic images of the breast (tomosynthesis) or perform an MRI. - Ultrasound
In addition to mammography, an ultrasound examination (high-resolution sonography) is carried out. This examination procedure can provide additional information on the extent and location of the findings. Ultrasound often provides better results, particularly in women with very dense glandular tissue. As a rule, a combination of mammography and ultrasound is recommended to clarify tumors. - Magnetic resonance imaging (MRI)
An MRI of the breast can also be carried out for special questions or in intensified early detection/follow-up care. This very special examination can provide information about the presence of multiple tumor foci or tumor foci hidden by mammography and sonography. - Tissue biopsy
If the patient has a palpable lump or a finding is visible on ultrasound, a tissue sample can be taken from the lump on an outpatient basis with a thin needle under local anesthesia for a histological examination. If the mammogram reveals conspicuous microcalcifications, for example, a sample can be taken under X-ray. The result is usually available within five working days. For subsequent control of the biopsy area, the physician can place a tiny titanium clip on the sampling site during the tissue removal. Depending on the results of the histological examination, the findings are discussed in detail with all experts in the tumor conference. Subsequently, the patient will usually be consulted about the further procedure approximately one week later. We ask the patient to remember to discontinue all blood-thinning medication one week before a planned tissue sample is taken after consulting her family physician or gynecologist - Staging (spread diagnostics)
If there is an increased risk of the tumor spreading (metastases), staging is carried out in accordance with the guidelines. The liver and lungs are examined using computer tomography (CT) and a bone scintigraphy is carried out to clarify the bones.
Close cooperation between surgeons and oncologists, pathologists, radiologists and radiotherapists is aprerequisite for the optimal planning and implementation of breast cancer treatment. Today, the procedure is highly individualized and takes into account the needs of the individual patient, the results of the physical examination and imaging diagnostics (mammography, sonography, MRI, X-ray, scintigraphy) and the results of the histological examination (histology).
At the first appointment at our Breast Center, the attending physician will discuss your medical history, your current illness and the possible examination steps in detail with the patient. This is followed by a palpation examination as well as an ultrasound and, if necessary, a mammography examination of the breast and lymph drainage channels. Further examinations may be carried out if specific questions arise:
The therapeutic procedure with regard to the disease is coordinated for the patients in the tumor conference, an interdisciplinary group of specialists. Specialists from the fields of surgical and oncological gynecology, internal oncology, radiology, radiotherapy, nuclear medicine and pathology discuss the diagnosis and individual treatment of patients on a weekly basis. This enables us to offer patients high-quality treatment and participation in clinical studies and to immediately incorporate the latest findings into diagnosis and treatment. The tumor conference protocol serves as the basis for a subsequent detailed information and consultation with the patient.
The three pillars of treatment for primary (non-metastatic) breast cancer consist of surgical therapy, systemic therapies and radiotherapy.
In the metastatic situation (spread to other organs), we speak of a chronic disease and systemic therapies are in the foreground in order to delay further progression of the disease. At the same time, the therapies should also aim to maintain quality of life.
Physicians in private practice are welcome to participate in the tumor conference, and patients can also be presented for joint consultation in this setting.
Breast surgery
Our experienced surgeons at the Breast Centre specialize in maintaining or restoring the natural shape of the breast in the case of tumours. The individual choice of surgical procedure is determined by the size and location of the tumor, the size and shape of the breast and, of course, the patient's wishes.
There are basically three different procedures:
- Breast-conserving therapy (BET), i.e. removal of the tumor tissue from the breast with the necessary safety margin,
- Removal of the entire mammary gland tissue (ablation),
- removal of the mammary gland tissue, combined with reconstruction (immediately or at a later date).
Whenever medically possible and responsible, we try to perform organ-preserving breast surgery. This is successful in around 70% of cases. Local tumor control and the chances of recovery must not be compromised. It is important to emphasize that subsequent radiation of the mammary gland is necessary in the case of a breast-preserving procedure. If the tumor is large or the primary size ratio of the tumor to the breast is unfavorable, the tumor can be reduced in size by means of neoadjuvant hormone and/or chemotherapy and breast-conserving therapy can then be attempted.
Breast-conserving surgery is not always possible in the treatment of breast cancer - depending on the type, extent and location of the tumor, the breast may have to be removed completely in some cases.
Here we can offer the entire spectrum of plastic reconstruction surgery, which includes implant-based breast reconstruction as well as breast reconstruction using the patient's own tissue. We work closely with our plastic surgery colleagues on an interdisciplinary basis. In our interdisciplinary consultation hours, we (gynecologist and plastic surgeon) advise the patient together in a detailed discussion. If there is a desire for breast reconstruction, the individualized treatment is developed together with the patient and a joint surgical concept is determined.
- Sentinel lymph node removal (differentiated surgery of the axilla, targeted axilla)
One component of surgical treatment is the removal of individual lymph nodes from the armpit of the affected side. The detection of tumor cells in the lymph nodes has a significant influence on further treatment planning. Here we use the so-called sentinel lymph node technique with the aim of minimizing complications with the affected arm. For this purpose, only individual lymph nodes are marked and thus removed in a targeted and gentle manner. Until now, a radioactive substance has always been used for this. A newer method is the use of Magtrace®. This is a substance that is detected with the help of a magnetic probe without any radiation. We can offer this safe and approved method to patients. If the lymph nodes are free of tumor cells, the other lymph nodes can be left in place.
Furthermore:
- Defect coverage by means of local skin displacement
- High proportion of oncoplastic breast reductions as part of tumor removal
- Prophylactic surgery for genetic disposition (after prior genetic counseling) in cooperation with plastic surgeons
We draw up a comprehensive oncoplastic concept with the patient as soon as the diagnosis is communicated. This includes the initiation of genetic counseling if necessary, the preparation of an expert opinion for submission to the health insurance company if necessary, the operation and post-operative care.
If an asymmetry of the breast occurs during breast-conserving surgery, a soft silicone compensation shell can compensate for this.
However, the healthy breast can also be reduced in size later on (corrective reduction surgery). Sometimes it is necessary to remove the nipple as well. To reconstruct a nipple, it is sculpted from surrounding skin or transplanted skin. After waiting for the healing process to complete, the patient can achieve the natural coloration of the areola with a tattoo.
A non-surgical option for breast reconstruction is a prosthesis in a bra or swimsuit. It is placed in a special pocket of the bra. As part of the inpatient stay, our affiliated medical supply store will initiate the first steps of treatment.
A soft, lightweight prosthesis made of fine microfiber fabrics and cotton is comfortable to wear immediately after breast removal. Soft silicone prostheses in individual shapes are available for full reconstruction.
Breast reconstruction can be performed immediately after tumor or breast removal or in a second operation at a later date. Reconstruction can be carried out using implants or the patient's own tissue. A combination of both techniques is also possible. The costs are covered by health insurance.
Most frequently - in around 75 percent of cases - the reconstruction is carried out using silicone implants by the specialist surgeons at our breast center if the skin envelope is sufficient. The prerequisite for this procedure is a sufficient soft tissue mantle with a good blood supply.
- One-stage procedure: If there is a sufficient skin mantle, a final silicone implant can be inserted during the same procedure as the breast removal. During the operation, the entire mammary gland is first removed while preserving the skin mantle. Whether the nipple-areola complex is preserved or removed depends on the location of the breast cancer. Whether the prosthesis is placed in front of or behind the pectoral muscle and support by a mesh is necessary depends on individual patient factors and is discussed in detail during the preliminary consultation.
- Two-stage procedure: This procedure is recommended in certain situations, e.g. if partial removal of the skin is necessary. In the first operation, an expander prosthesis is implanted first. After the operation, it is gradually filled with saline solution via a valve. As soon as a breast size suitable for the patient is achieved, the expander is removed in a second operation and the final silicone prosthesis is implanted in its place.
Disadvantages: It should be borne in mind that the lifespan of implants can be limited by the occurrence of a wound healing disorder or painful capsular fibrosis (hardened encapsulation of the implant with deformation of the breast). A defect in the prosthesis shell can also occur as the implant ages, meaning that the implant must then be removed or replaced. The risk of such complications is increased by radiotherapy and is up to 60 percent. Therefore, if radiotherapy is necessary, reconstruction using the patient's own tissue should be considered.
If certain conditions for reconstruction using an implant are not met and/or reconstruction with foreign material is not desired, a breast can be reconstructed using the body's own tissue without foreign materials.
The advantages of reconstruction with the patient's own tissue are that no implant complications such as an aged and defective implant or capsular fibrosis can develop, and a long-term stable end result can be achieved.
On the other hand, augmentation using autologous tissue is significantly more complex, the body needs a much longer recovery time and large scars occur in the area of the donor sites. In addition, movement restrictions may occur if parts of the muscles (abdomen or back) are used.
The autologous tissue methods include skin and muscle tissue from the back (latissimus dorsi flap), but nowadays a free flap plasty with skin and fatty tissue from the lower abdomen (DIEP = deep inferior epigastric perforator flap) is performed much more frequently. The abdominal muscles remain intact with this method. Like the latissimus dorsi flap, the pedicled flap using the TRAM flap (Transverse Rectus Abdominis Muscle) has the disadvantage that muscles are also used for this. This can lead to a severe weakening of the abdominal wall. Other tissue grafts from other regions of the body (inner thigh, posterior flank) are available.
In our plastic-senology consultation, we advise patients jointly (gynecologist and plastic surgeon) on all forms of breast reconstruction. The planning and execution of the operation is then also carried out jointly.
The type of follow-up treatment depends on the size of the tumor, the tumor biology and any lymph node involvement. Additional anti-hormonal therapy, antibody therapy, chemotherapy and/or radiotherapy may be required. Based on more precise knowledge of the various forms of breast cancer, science has now also developed so-called "targeted therapy", i.e. targeted therapies, which are included in our standard treatment recommendations. In certain cases, special test procedures, such as the Oncotype DX test, can be used to determine whether chemotherapy is necessary. A genetic cause of the breast cancer is also taken into account when selecting the medication.
These treatments are carried out on an outpatient basis in our gynecological oncology department.
This might interest you
ResearchAnother focus is on the further development of the field. In the research area of the Women's Clinic, we are dedicated to basic scientific and translational issues.
StudiesWe also offer clinical studies on breast cancer.
Drug oncology | Chemotherapy outpatient clinic
In gynecological-oncological treatment, we now have a range of modern therapeutic procedures at our disposal. In addition to surgical therapy, drug therapy (e.g. chemotherapy, targeted therapy or immunotherapy) has also become very important.