Project presentation 2024
3D PREFUL-MRI for visualization and quantification of regional lung function
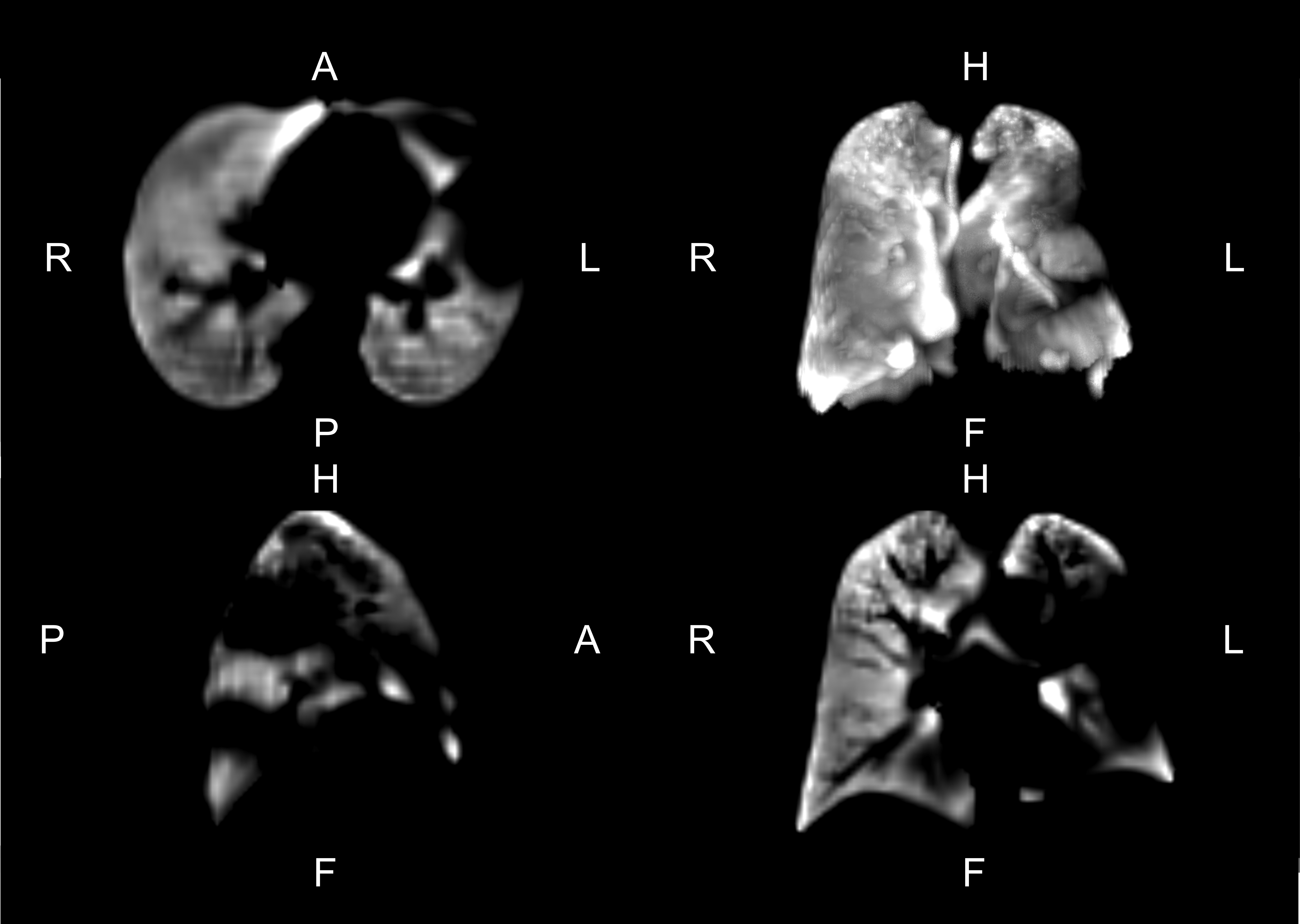
In recent years, a novel 2D MRI method (PREFUL: Phase-Resolved Functional LungMRI) for dynamic visualization and quantification of regional lung ventilation and perfusion without contrast agent has been invented, validated and applied in clinical studies in the working group of Prof. Dr. Jens Vogel-Claussen at the Institute of Diagnostic and Interventional Radiology with funding from the German Center for Lung Research (DZL ). PREFUL uses the intrinsic signal alterations caused by breathing and the heartbeat during data processing after the MRI examination. To date, PREFUL-MRI has been shown to be sensitive for early assessment of treatment response in patients with chronic obstructive pulmonary disease (COPD), cystic fibrosis (CF), asthma and COVID-19 and early prediction of chronic lung transplant failure. The 3D MRI-PREFUL method was developed to capture the entire lung volume without gaps. Commercially available MRI sequences are used to enable the scalability of the PREFUL method.
In this validation study, the ventilation maps obtained from the 3D-PREFUL MRI are compared with a direct ventilation measurement from the 129Xe MRI (gold standard) in patients with COPD and healthy volunteers. This study was conducted in collaboration with Fraunhofer ITEM.
Thirty-one COPD patients and 12 healthy controls underwent free-breathing 3D-PREFUL MRI and 129Xe MRI. Ventilation defect (VD) maps were created for both MRI techniques and the corresponding values for the percentage of ventilation defects (VDP) were calculated. All parameters of both techniques were compared using the Spearman correlation coefficient (r). The differences between the VDP values were quantified using Bland-Altman analysis and tested using the Wilcoxon signed rank test. In a regional comparison of the VD maps, the spatial overlap and Sørensen-Dice coefficients of healthy and defective areas were calculated.
On a global scale, both static (RVent) and 3D PREFUL VDP values derived from dynamic flow-volume curves (FVL-CM) correlated significantly with the VDP value derived from 129Xe ventilation imaging (all r > 0.65; all p < 0.0001). 129Xe VDP was significantly greater than 3D PREFUL-derived VDPRVent (mean deviation = 10.5%, p < 0.001) and VDPFVL-CM (mean deviation = 11.3%, p < 0.0001), but not for VDPCombined - a combination of RVent and FVL-CM (mean deviation = 1.7%, p = 0.70). The overall regional agreement of the 129Xe and 3D-PREFUL-VD maps was between 60 % and 63 %.
Free-breathing 3D-PREFUL MRI showed a strong correlation with breath-hold hyperpolarized 129Xe MRI in terms of VDP values and slight differences in the detection of VDs at the regional level. This work is an important step for the clinical translation of 3D PREFUL MRI.
Publication
Free-breathing 3D phase-resolved functional lung MRI vs breath-hold hyperpolarized 129Xe ventilation MRI in patients with chronic obstructive pulmonary disease and healthy volunteers
Klimeš F, Kern AL, Voskrebenzev A, Gutberlet M, Grimm R, Müller RA, Behrendt L, Kaireit TF, Glandorf J, Alsady TM, Wacker F, Hohlfeld JM, Vogel-Claussen J.
Further information
Publisher:
President of the Hannover Medical School
Univ.-Prof. Dr. Denise Hilfiker-Kleiner, Ph.D.
Dean of Research at Hannover Medical School
Prof. Dr. med. dent. Meike Stiesch
Processing and contact person:
Reporting department of the Hannover Medical School
Alica Wollmann
Phone: 0511/ 532- 5578
E-mail: wollmann.alica@mh-hannover.de
Online implementation:
Office of the Dean of Research at Hannover Medical School
Jan Tauwaldt
and
Reporting Department of Hannover Medical School
Alica Wollmann
Phone: 0511/ 532- 5578
Research report 2024
Here you can find the research report created with the help of the Research Information System (FIS). As in previous years, we would like to take the opportunity here to explicitly present one project as a representative.
Research Information System (FIS)Here you can find further information on the Research Information System (FIS).
University bibliography- Project presentation 2023
- Project presentation 2022
- Project presentation 2021
- Project presentation 2020
- Project presentation 2019
- Project presentation 2018
- Project presentation 2017
- Research report 2016
- Research report 2015
- Research report 2014
- Research report 2013
- Research report 2012
- Research report 2011
- Research Report 2010
- Research Report 2009
- Research Report 2008
- Research Report 2007